Aspergilloma
Updates to Article Attributes
Aspergillomas are mass-like fungus balls that are typically composed of Aspergillusfumigatus, and are a a non-invasive form of pulmonary aspergillosis.
Terminology
Although the term 'mycetoma' is is frequently used to describe these fungal balls, it is an incorrect term to use5-6.
Epidemiology
Aspergillomas occur in patients with normal immunity but structurally abnormal lungs, with pre-existing cavities. Demographics will therefore match those of the underlying condition, such as2:
- pulmonary tuberculosis: most common, accounting for 25-80% of cases depending on the prevalence of TB in the population 2-3
- pulmonary sarcoidosis
- bronchiectasis from any cause
- other pulmonary cavities
- bronchogenic cyst 4
- pulmonary sequestration
- PJP associatedpneumatocoeles
Clinical presentation
Most aspergillomas are asymptomatic. Occasionally due to surrounding reactive vascular granulation tissue, haemoptysis may be present. Occasionally, erosion into a bronchial artery may lead to life-threatening haemoptysis1.
Pathology
An aspergilloma is a mass-like collection of fungal hyphae, mixed with mucus and cellular debris, within a cavity the walls of which demonstrate vascular granulation tissue1-2.
Distribution
Aspergillomas typically occur in the cavities of post-primary pulmonary tuberculosis. Therefore, they most frequently are found in the posterior segments of the upper lobes and the superior segments of the lower lobes.
Radiographic features
A mycetoma can be seen on both plain film and CT as an intracavitary mass surrounded by a crescent of air. The term "air-crescent" is however really seen in recovering invasive pulmonary aspergillosis. It is wrongly used by many to describe the air around an aspergilloma. The correct term to describe describe the cresent of air is the Monad sign in the setting of aspergilloma developing in a preexisting cavity, although it is less widely recognised.
Plain film
Aspergillomas typically appear as rounded or ovoid soft tissue attenuating masses located in a surrounding cavity and outlined by a crescent of air1-4. Altering the position of the patient usually demonstrates that the mass is mobile, thus confirming the diagnosis.
CT
Appearances are those of a well formed cavity with a central soft tissue attenuating rounded mass surrounded by an cresent of air (Monad sign). The mass is typically spherical or ovoid. On different positioning of the patient, the mass can be shown to be mobile. On occasion the mass may entirely fill the cavity, thus taking on the shape of the cavity, obliterating the surrounding air crescent and no longer being mobile2.
Calcification is not uncommon, which can range from none to heavy. Due to the inflammation and vascular granulation tissue formation, the bronchial arteries supplying the supplying the wall can sometimes be seen as markedly enlarged2.
The adjacent pleura may well be thickened.
Treatment and prognosis
An asymptomatic aspergilloma does not necessarily require treatment, and the cavity is essentially isolated from any systemic administration of anti-fungals3.
In the setting of brisk haemoptysis, angiography may be performed on an emergency basis and selective bronchial artery embolisation can be life saving. Failing this, or in cases of repeated haemoptysis surgical excision with a lobectomy remains the gold standard3.
Mortality rate varies widely, but in more recent series is low, even where requiring surgery3.
Differential diagnosis
When classical in appearance there is little differential. If the mass fills the cavity completely then the differential is that of solitary pulmonary nodule.
See also
-<p><strong>Aspergillomas</strong> are mass-like fungus balls that are typically composed of <em><a href="/articles/aspergillus-fumigatus">Aspergillus fumigatus</a></em>, and are a non-invasive form of <a href="/articles/pulmonary-aspergillosis">pulmonary aspergillosis</a>. Although the term '<a href="/articles/mycetoma">mycetoma</a>' is frequently used to describe these fungal balls, it is an incorrect term to use <sup>5-6</sup>.</p><h4>Epidemiology</h4><p>Aspergillomas occur in patients with normal immunity but structurally abnormal lungs, with pre-existing cavities. Demographics will therefore match those of the underlying condition, such as <sup>2</sup>:</p><ul>- +<p><strong>Aspergillomas</strong> are mass-like fungus balls that are typically composed of <em><a href="/articles/aspergillus-fumigatus">Aspergillus fumigatus</a></em>, and are a non-invasive form of <a href="/articles/pulmonary-aspergillosis">pulmonary aspergillosis</a>.</p><h4>Terminology</h4><p>Although the term <strong><a href="/articles/mycetoma">mycetoma</a></strong> is frequently used to describe these fungal balls, it is an incorrect term to use <sup>5-6</sup>.</p><h4>Epidemiology</h4><p>Aspergillomas occur in patients with normal immunity but structurally abnormal lungs, with pre-existing cavities. Demographics will therefore match those of the underlying condition, such as <sup>2</sup>:</p><ul>
-<a href="/articles/pulmonary-manifestations-of-tuberculosis">pulmonary tuberculosis</a>: most common, accounting for 25-80% of cases depending on the prevalence of TB in the population <sup>2-3</sup>- +<a href="/articles/tuberculosis-pulmonary-manifestations">pulmonary tuberculosis</a>: most common, accounting for 25-80% of cases depending on the prevalence of TB in the population <sup>2-3</sup>
-<a href="/articles/pneumocystis-pneumonia">PJP</a> associated <a href="/articles/pneumatocoeles">pneumatocoeles</a>- +<a href="/articles/pneumocystis-pneumonia">PJP</a> associated <a href="/articles/pneumatocoeles">pneumatocoeles</a>
-</ul><h4>Clinical presentation</h4><p>Most aspergillomas are asymptomatic. Occasionally due to surrounding reactive vascular granulation tissue, <a href="/articles/haemoptysis-1">haemoptysis</a> may be present. Occasionally, erosion into a bronchial artery may lead to life-threatening haemoptysis <sup>1</sup>.</p><h4>Pathology</h4><p>An aspergilloma is a mass-like collection of fungal hyphae, mixed with mucus and cellular debris, within a cavity the walls of which demonstrate vascular granulation tissue <sup>1-2</sup>.</p><h5>Distribution</h5><p>Aspergillomas typically occur in the cavities of <a href="/articles/pulmonary-manifestations-of-tuberculosis">post-primary pulmonary tuberculosis</a>. Therefore, they most frequently are found in the posterior segments of the upper lobes and the superior segments of the lower lobes.</p><h4>Radiographic features</h4><p>A mycetoma can be seen on both plain film and CT as an intracavitary mass surrounded by a crescent of air. The term "air-crescent" is however really seen in recovering invasive pulmonary aspergillosis. It is wrongly used by many to describe the air around an aspergilloma. The correct term to describe the cresent of air is the <a href="/articles/monad-sign">Monad sign</a> in the setting of aspergilloma developing in a preexisting cavity, although it is less widely recognised.</p><h5>Plain film</h5><p>Aspergillomas typically appear as rounded or ovoid soft tissue attenuating masses located in a surrounding cavity and outlined by a crescent of air <sup>1-4</sup>. Altering the position of the patient usually demonstrates that the mass is mobile, thus confirming the diagnosis.</p><h5>CT</h5><p>Appearances are those of a well formed cavity with a central soft tissue attenuating rounded mass surrounded by an cresent of air (<a href="/articles/monad-sign">Monad sign)</a>. The mass is typically spherical or ovoid. On different positioning of the patient, the mass can be shown to be mobile. On occasion the mass may entirely fill the cavity, thus taking on the shape of the cavity, obliterating the surrounding air crescent and no longer being mobile <sup>2</sup>.</p><p>Calcification is not uncommon, which can range from none to heavy. Due to the inflammation and vascular granulation tissue formation, the bronchial arteries supplying the wall can sometimes be seen as markedly enlarged <sup>2</sup>.</p><p>The adjacent pleura may well be thickened.</p><h4>Treatment and prognosis</h4><p>An asymptomatic aspergilloma does not necessarily require treatment, and the cavity is essentially isolated from any systemic administration of anti-fungals <sup>3</sup>.</p><p>In the setting of brisk haemoptysis, angiography may be performed on an emergency basis and selective bronchial artery embolisation can be life saving. Failing this, or in cases of repeated haemoptysis surgical excision with a lobectomy remains the gold standard <sup>3</sup>.</p><p>Mortality rate varies widely, but in more recent series is low, even where requiring surgery <sup>3</sup>.</p><h4>Differential diagnosis</h4><p>When classical in appearance there is little differential. If the mass fills the cavity completely then the differential is that of <a href="/articles/solitary-pulmonary-nodule-2">solitary pulmonary nodule</a>.</p><h4>See also</h4><ul><li><a href="/articles/causes-of-an-air-crescent-sign">causes of an air crescent sign</a></li></ul>- +</ul><h4>Clinical presentation</h4><p>Most aspergillomas are asymptomatic. Occasionally due to surrounding reactive vascular granulation tissue, <a href="/articles/haemoptysis-1">haemoptysis</a> may be present. Occasionally, erosion into a bronchial artery may lead to life-threatening haemoptysis <sup>1</sup>.</p><h4>Pathology</h4><p>An aspergilloma is a mass-like collection of fungal hyphae, mixed with mucus and cellular debris, within a cavity the walls of which demonstrate vascular granulation tissue <sup>1-2</sup>.</p><h5>Distribution</h5><p>Aspergillomas typically occur in the cavities of <a href="/articles/tuberculosis-pulmonary-manifestations">post-primary pulmonary tuberculosis</a>. Therefore, they most frequently are found in the posterior segments of the upper lobes and the superior segments of the lower lobes.</p><h4>Radiographic features</h4><p>A mycetoma can be seen on both plain film and CT as an intracavitary mass surrounded by a crescent of air. The term "air-crescent" is however really seen in recovering invasive pulmonary aspergillosis. It is wrongly used by many to describe the air around an aspergilloma. The correct term to describe the cresent of air is the <a href="/articles/monod-sign-1">Monad sign</a> in the setting of aspergilloma developing in a preexisting cavity, although it is less widely recognised.</p><h5>Plain film</h5><p>Aspergillomas typically appear as rounded or ovoid soft tissue attenuating masses located in a surrounding cavity and outlined by a crescent of air <sup>1-4</sup>. Altering the position of the patient usually demonstrates that the mass is mobile, thus confirming the diagnosis.</p><h5>CT</h5><p>Appearances are those of a well formed cavity with a central soft tissue attenuating rounded mass surrounded by an cresent of air (<a href="/articles/monod-sign-1">Monad sign)</a>. The mass is typically spherical or ovoid. On different positioning of the patient, the mass can be shown to be mobile. On occasion the mass may entirely fill the cavity, thus taking on the shape of the cavity, obliterating the surrounding air crescent and no longer being mobile <sup>2</sup>.</p><p>Calcification is not uncommon, which can range from none to heavy. Due to the inflammation and vascular granulation tissue formation, the bronchial arteries supplying the wall can sometimes be seen as markedly enlarged <sup>2</sup>.</p><p>The adjacent pleura may well be thickened.</p><h4>Treatment and prognosis</h4><p>An asymptomatic aspergilloma does not necessarily require treatment, and the cavity is essentially isolated from any systemic administration of anti-fungals <sup>3</sup>.</p><p>In the setting of brisk haemoptysis, angiography may be performed on an emergency basis and selective bronchial artery embolisation can be life saving. Failing this, or in cases of repeated haemoptysis surgical excision with a lobectomy remains the gold standard <sup>3</sup>.</p><p>Mortality rate varies widely, but in more recent series is low, even where requiring surgery <sup>3</sup>.</p><h4>Differential diagnosis</h4><p>When classical in appearance there is little differential. If the mass fills the cavity completely then the differential is that of <a href="/articles/solitary-pulmonary-nodule-2">solitary pulmonary nodule</a>.</p><h4>See also</h4><ul><li><a href="/articles/causes-of-an-air-crescent-sign">causes of an air crescent sign</a></li></ul>
Image ( destroy )
Image ( destroy )
Image 11 CT (lung window) ( update )
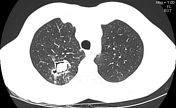
Image 12 CT (lung window) ( update )

Image 13 CT (lung window) ( update )

Image 14 CT (lung window) ( update )

Image 15 CT (lung window) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.