Demyelination vs. dysmyelination.
Demyelination (adults): acquired disorder that affects normal myelin
Dysmyelination (children): inherited disorder affecting the formation or maintenance of myelin (rare)
Dysmyelination:
-
Primary
-
Multiple sclerosis
- Age: 20-40
- Multiple CNS lesions separated in time & space
- Histopath: inflammation (separates MS from other WM conditions such as PRES, osmotic myelinolysis), perivenular inflammation
- Location:
- Periventricular white matter
- Corpus callosum
- Cerbellum
- Spine
- Perivenular, juxtacortical -> round/ovoid
- High T2 -> active inflammation or chronic scarring
- Enhancing & abnormal diffusion restriction = acute lesions
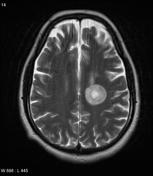
- Subtype = tumefactive MS
- Large, conglomerate mass (can be difficult to differentiate from malignancy)
- Open ring enhancement -> leading edge of demyelination
-
Multiple sclerosis
-
Ischaemic (OLD > 50 yrs)
-
Deep white matter infarcts
- Deep cerebral and periventricular white matter
- Cortex, subcortical U fibres, corpus callosum, medulla, midbrain, cerebellar peduncles are usually spared
- Deep cerebral and periventricular white matter
- Lacunar infarcts
- 5-10 mm within basal ganglia (upper 2/3 of putamina)
- Vasculitis (sarcoidosis & lupus)
- Dissection
- Migrainous ischaemia
- Moyamoya disease
- CADASIL = cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy
- Inherited (notch3 mutation)
- Subcortical anterior temporal and medial frontal lesions (relatively specific)
- Presents middle age
-
Deep white matter infarcts
Prominent perivascular space can mimic deep whit matter/ lacunar infarcts -> u
3. Infectious
-
Progressive multifocal leukoencephalopathy
- Immunocompromised
- Reactivation of latent JC virus
- Deep cerebral WM, subcortical U-fibres -> spares cortex and deep grey matter
- No mass affect, haemorrhage or contrast enhancement
- Coalesce
- HIV encephalopathy
- Mild cerebral atrophy without focal abnormality
- Herpes encephalopathy
- Temporal lobes, insular cortex, subfrontal area and cingulate gyro
- Haemorrhage within area of involved parenchyma is strongly supportive of diagnosis
- ADEM
- Post-infective & post-vaccination -> viral illnesses approximately 2 weeks later
- Children
- Multifocal or confluent WM lesions (can also involve grey matter) -> monophasic (compared to MS)
- Hursts disease = haemorrhagic subtype
- Subacute sclerosing panencephalitis -> measles ((age 5-12)
- Lyme disease
- Neurosyphilis
4. Toxic & Metabolic
-
Central pontine myelinolysis
- Characteristic demyelination of pons
- Patients with electrolyte abnormalities (children & alcoholics w malnutrition)
- Biphasic
- Rapidly evolving corticospinal syndrome with quadriplegia
- Also involves thalamus, BG
- PRES = posterior reversible encephalopathy syndrome
- Symmetric bilateral subcortical and cortical vasogenic oedema within the parietooccipital lobes
- Marchiafava-Bignami disease (rare)
- Demyelination of the central fibres of the CC
- Form of osmotic demyelination
- Wernicke-Korsakoff syndrome (thiamine B1)
- Acute: High T2/enhancement of maxillary bodies, BG, thalamus & brainstem
- Radiation injury
- History of radiotherapy
- Toxic leukoencephalopathy -> chasing the dragon
- Symmetrical involvement
- Subcortical u fibres spared
- Butterfly wing pattern of cerebellar WM
5. Dysmyelination
- Metachromatic leukodystrophy
- Adrenal leukodystrophy
- Leigh disease
- Alexander disease


















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.