Benign and malignant characteristics of breast lesions at ultrasound
Updates to Article Attributes
BreastBenign and malignant characteristics of breast lesions at ultrasound have a number of characteristics which allowsallow the classification as either malignant, intermediate or benign. In 1995, A. Thomas based on work published by Stavros published an important paperet al in Radiology1995 1 which established the usefulness of various ultrasound.
Radiographic features in distinguishing benign from malignant lesions.
US
Malignant characteristics (with positive predictive values)
-
sonographic spiculation: 87-90% 1,4
:-
alternate hypo-hyperechoic lines radiating perpendicularly from surface of nodules
(If(if lesion is surrounded by echogenic tissue,youhypoechoic strands willsee hypoechoic strands. Ifbe seen; if lesion is surrounded by fat, echogenic strands may be seen).
-
alternate hypo-hyperechoic lines radiating perpendicularly from surface of nodules
- deeper (taller) than wide: 74-80% 1,4
:-
except in certain grade III Invasive ductal carcinomas
.
-
except in certain grade III Invasive ductal carcinomas
-
microlobulations: 75%
:- small lobulations 1
- 2-2 mm on the surface; risk of malignancy rises with increasing numbers.
- small lobulations 1
- thick hyperechoic halo: 74 %
- angular margins: 70%
- markedly hypoechoic nodule: 70%
- sonographic posterior accoustic shadowing: 50%
- branching pattern: 30%
:- multiple projections from the nodule within or around ducts extending away from the nipple, usually seen in larger tumours
.
- multiple projections from the nodule within or around ducts extending away from the nipple, usually seen in larger tumours
- punctate calcifications: 25%
:- which usually do not shadow
.
- which usually do not shadow
- duct extension: 25%
:- is seen as projection from a nodule which extends radially within or around a duct towards the nipple
- heterogeneous echotexture 3
- compressibility:
- in general terms, benign lesions compress with transducer pressure and malignant lesions displace the breast tissue without changing in height
. This; this is the basis for elastography.
- in general terms, benign lesions compress with transducer pressure and malignant lesions displace the breast tissue without changing in height
Benign characteristics (with negative predictive values)
- well circumscribed, hyperechoic tissue:
~ 100~100% - wider than deep: 99%
- gently curving smooth lobulations (<3 in a wider than deep nodule, i.e. D/W ratio <1): 99%
-
thin echogenic pseudocapsule in a wider than deep nodule: 99%
. It-
it is best seen on anterior
/ posterior/posterior margins, perpendicular to the beam. It - probably represents normal compressed tissue consistent with a non infiltrative process
.
-
it is best seen on anterior
Treatment and prognosis
In all cases of lesions other than absolutely benign, real time review by the radiologist is mandatory. Review of the mammogram is essential when interpretation of an ultrasound is done. In those under 30 year old, ultrasound is the primary imaging modality. In those over 40, both modalities are performed and interpretted in tandem.
Any lesion classified as benign must be benign on both modalities.
Further work upworkup strategy
- if there is a single malignant feature >> consider biopsy
- if there are no malignant features >> then look for benign features
- if there are no malignant features or any benign features >> indeterminate
:- consider biopsy - look at the mammogram
.
Practical considerations
In all cases of lesions other than absolutely benign, real time review by the radiologist is mandatory. Review of the mammogram is essential when interpretation of an ultrasound is done. In those under 30 years, ultrasound is the primary imaging modailty. In those over 40, both modalities are performed and interpretted in tandem.
Any lesion classified as benign must be benign on both modalities.
See also
-<p><strong>Breast lesions at ultrasound</strong> have a number of characteristics which allows the classification as either malignant, intermediate or benign. In 1995, A. Thomas Stavros published an important paper in Radiology <sup>1</sup> which established the usefulness of various ultrasound features in distinguishing benign from malignant lesions.</p><h5>Malignant characteristics (with positive predictive values)</h5><ul>- +<p><strong>Benign and malignant characteristics of breast lesions at ultrasound</strong> allow the classification as either malignant, intermediate or benign based on work published by Stavros et al in 1995 <sup>1</sup>.</p><h4>Radiographic features</h4><h5>US</h5><h6>Malignant characteristics (with positive predictive values)</h6><ul>
-<a href="/articles/sonographic-spiculation">sonographic spiculation</a>: 87-90% <sup>1,4</sup> : alternate hypo-hyperechoic lines radiating perpendicularly from surface of nodules (If lesion is surrounded by echogenic tissue, you will see hypoechoic strands. If lesion is surrounded by fat, echogenic strands may be seen).</li>-<li>deeper (taller) than wide: 74-80% <sup>1,4 </sup>: except in certain grade III Invasive ductal carcinomas.</li>-<li>-<a href="/articles/microlobulations">microlobulations</a>: 75% : small lobulations 1 - 2 mm on the surface; risk of malignancy rises with increasing numbers.</li>-<li>-<strong>thick </strong>hyperechoic halo: 74 %</li>- +<a href="/articles/sonographic-spiculation">sonographic spiculation</a>: 87-90% <sup>1,4</sup><ul><li>
- +<sup></sup>alternate hypo-hyperechoic lines radiating perpendicularly from surface of nodules (if lesion is surrounded by echogenic tissue, hypoechoic strands will be seen; if lesion is surrounded by fat, echogenic strands may be seen</li></ul>
- +</li>
- +<li>deeper (taller) than wide: 74-80% <sup>1,4 </sup><ul><li>
- +<sup></sup>except in certain grade III Invasive ductal carcinomas</li></ul>
- +</li>
- +<li>
- +<a href="/articles/microlobulations">microlobulations</a>: 75%<ul><li>small lobulations 1-2 mm on the surface; risk of malignancy rises with increasing numbers</li></ul>
- +</li>
- +<li>thick hyperechoic halo: 74 %</li>
-<li>branching pattern: 30% : multiple projections from the nodule within or around ducts extending away from the nipple, usually seen in larger tumours.</li>-<li>punctate calcifications: 25% : which usually do not shadow.</li>-<li>duct extension: 25% : is seen as projection from a nodule which extends radially within or around a duct towards the nipple</li>- +<li>branching pattern: 30%<ul><li>multiple projections from the nodule within or around ducts extending away from the nipple, usually seen in larger tumours</li></ul>
- +</li>
- +<li>punctate calcifications: 25%<ul><li>which usually do not shadow</li></ul>
- +</li>
- +<li>duct extension: 25%<ul><li>is seen as projection from a nodule which extends radially within or around a duct towards the <a title="Nipple-areola complex" href="/articles/nipple-areola-complex">nipple</a>
- +</li></ul>
- +</li>
-<li>compressibility: in general terms, benign lesions compress with transducer pressure and malignant lesions displace the breast tissue without changing in height. This is the basis for<a href="/articles/elastography"> elastography</a>.</li>-</ul><p> </p><h5>Benign characteristics (with negative predictive values)</h5><ul>-<li>well circumscribed, hyperechoic tissue: ~ 100%</li>- +<li>compressibility:<ul><li>in general terms, benign lesions compress with transducer pressure and malignant lesions displace the breast tissue without changing in height; this is the basis for<a href="/articles/elastography"> elastography</a>
- +</li></ul>
- +</li>
- +</ul><h6>Benign characteristics (with negative predictive values)</h6><ul>
- +<li>well circumscribed, hyperechoic tissue: ~100%</li>
-<li>gently curving smooth lobulations (<3 in a wider than deep nodule, i.e. D/W ratio <1) : 99%</li>-<li>-<strong>thin </strong>echogenic pseudocapsule in a wider than deep nodule : 99%. It is best seen on anterior / posterior margins, perpendicular to the beam. It probably represents normal compressed tissue consistent with a non infiltrative process.</li>-</ul><h5>Further work up strategy</h5><ul>- +<li>gently curving smooth lobulations (<3 in a wider than deep nodule, i.e. D/W ratio <1): 99%</li>
- +<li>thin echogenic pseudocapsule in a wider than deep nodule: 99%<ul>
- +<li>it is best seen on anterior/posterior margins, perpendicular to the beam</li>
- +<li>probably represents normal compressed tissue consistent with a non infiltrative process</li>
- +</ul>
- +</li>
- +</ul><h6><span style="font-size:1.5em; line-height:1em">Treatment and prognosis</span></h6><p>In all cases of lesions other than absolutely benign, real time review by the radiologist is mandatory. Review of the mammogram is essential when interpretation of an ultrasound is done. In those under 30 year old, ultrasound is the primary imaging modality. In those over 40, both modalities are performed and interpretted in tandem.</p><p>Any lesion classified as benign must be benign on both modalities.</p><h6>Further workup strategy</h6><ul>
-<li>if there are no malignant features or any benign features >> indeterminate : consider biopsy </li>-<li>look at the mammogram.</li>-</ul><h4>Practical considerations</h4><p>In all cases of lesions other than absolutely benign, real time review by the radiologist is mandatory. Review of the mammogram is essential when interpretation of an ultrasound is done. In those under 30 years, ultrasound is the primary imaging modailty. In those over 40, both modalities are performed and interpretted in tandem.</p><p>Any lesion classified as benign must be benign on both modalities.</p><h4>See also</h4><ul>- +<li>if there are no malignant features or any benign features >> indeterminate - consider biopsy </li>
- +<li>look at the mammogram</li>
- +</ul><h4>See also</h4><ul>
Image 1 Ultrasound ( update )

Image 2 Mammography (CC) ( update )

Image 3 Ultrasound ( update )
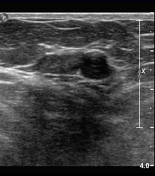
Image 4 Ultrasound (Transverse) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.