Brain arteriovenous malformation
Updates to Article Attributes
Brain arteriovenous malformations are type of intracranial high-flow vascular malformation composed of enlarged feeding arteries, a nidus of vessels closely associated with the brain parenchyma through which arteriovenous shunting occurs, and draining veins.
Terminology
This article corresponds to the classic form of arteriovenous malformation involving the brain parenchyma. The term brain arteriovenous malformation (BAVM) is the preferred term 12. An alternative is cerebral arteriovenous malformation (CAVM), but the term cerebral leaves out more caudal brain structures and the abbreviation could be confused with cavernous malformation. It is also referred to as a pial arteriovenous malformation if it is related to the pial vessels, but this is not always the case 6.
These malformations are characterised by a nidus forming the transition between the feeding artery and draining vein. If this transition is made directly, then it is considered an arteriovenous fistula, which is a separate type of cerebral vascular anomaly.
Epidemiology
Although arteriovenous malformations are thought to represent a congenital abnormality, they are rarely found incidentally in the very young and are thought to expand over time. Despite this, a third of arteriovenous malformations that are diagnosed due to haemorrhage are identified before the age of 20 years 7. Overall, they are diagnosed at a mean age of 31 years 8.
Arteriovenous malformations are thought to occur in approximately 4% of the population but become symptomatic in only 12% of affected individuals 8. There is no gender predilection 8.
AVMs tend to be solitary in the vast majority of cases (>95%). When multiple, syndromic associations must be considered, including:
- hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu syndrome)
- Wyburn-Mason syndrome (craniofacial arteriovenous metameric syndrome)
Clinical presentation
Cerebral arteriovenous malformations are the most common symptomatic vascular malformations. Possible presentations include 3:
- incidental finding in asymptomatic patients: 15% 5
- seizures: 20%
- headaches
- ischaemic events due to vascular steal from normal brain
- haemorrhage: 65% 5, incidence 2-3% per year 3
- parenchymal
- subarachnoid
- intraventricular
Pathology
The origin of arteriovenous malformations remains uncertain, although they are thought to be multifactorial and often attributed to being congenital 3. Their development may involve dysregulation of vascular endothelium growth factor (VEGF) receptor-mediated endothelial proliferation and cytokine-mediated vessel remodelling1.
Arteriovenous malformations comprise a number of components:
- feeding arteries
- nidus (Latin for "nest")
- shunting arterioles: the true culprit
- interconnected venous loops
- draining veins
The nidus is fed by one or more arteries and drained by one or more veins. The feeding arteries are enlarged due to the low resistance (as blood bypasses the capillary beds) and therefore increased flow, which may lead to flow-related arterial aneurysms 3. Venous aneurysms, also referred to as venous pouches, may be seen as well. AVMs may contain dystrophic calcification, a small amount of gliotic tissue, or blood at different stages of ageing.
Location
- supratentorial: ~85%
- superficial (two-thirds)
- deep (one-third)
- infratentorial: ~15%
Incidence
- solitary AVMs (98%)
- multiple AVMs (2%)
- often associated with syndromes
Associated abnormalities
- flow-related angiopathy secondary to endothelial hyperplasia
- flow-related aneurysm
- intranidal: located in the nidus
- intrapedicular: located in the feeding vessel
- remote aneurysm: haemodynamically unrelated to malformation
Classification and grading
Brain AVMs can be divided into two types 4,6:
- compact (or glomerular) nidus: abnormal vessels without any interposed normal brain tissue. More common than diffuse nidus type.
-
diffuse (or proliferative) nidus: no well-formed nidus is present, with functional neuronal tissue interspersed amongst the anomalous vessels.
- when early venous drainage is absent, this is considered cerebral proliferative angiopathy 6,9
The Spetzler-Martin AVM grading system relates morphology and location to the risk of surgery.
Radiographic features
CT
Diagnosis can be difficult on non-contrast CT. The nidus is blood density and therefore usually somewhat hyperdense compared to adjacent brain. Enlarged draining veins may be seen. Although they might be very large in size, they do not cause any mass effect unless they bleed.
Following contrast administration, and especially with CTA, the diagnosis is usually self-evident, with feeding arteries, draining veins, and intervening nidus visible in the so-called "bag of worms" appearance. The exact anatomy of feeding vessels and draining veins can be difficult to delineate, so angiography remains necessary.
Angiography (DSA)
Cerebral angiography remains the gold standard, able to exquisitely delineate the location and number of feeding vessels and the pattern of drainage. Ideally, angiography is performed in a bi-plane system with a high rate of acquisition, as shunting can be very rapid.
On angiography, an AVM appears as a tightly packed mass of enlarged feeding arteries that supply a central nidus. One or more dilated veins drain the nidus and abnormal opacification of veins occurs in the arterial phase (early venous drainage), represents shunting.
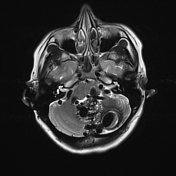
MRI
Fast flow generates flow voids, easily seen on T2 weighted images. Complications, including previous haemorrhage and adjacent oedema, may be evident.
- MRA: phase-contrast MR angiography is often useful for subtracting the haematoma components when an AVM complicated by an acute haemorrhage needs to be imaged.
Radiology reports should include certain key points that help the clinician in deciding the management. Radiological evidence of previous haemorrhage, intranidal aneurysm, ectasia or stenosis of draining veins, single draining vein or deep draining vein, or deep or posterior fossa location of AVM is associated with a high risk of future haemorrhage.6
Risk of non-haemorrhagic complications like focal neurological deficit increases with a long pial course of a draining vein, arterial steal, mass effect, and perinidal gliosis.6
Treatment and prognosis
Treatment options and rate of complications are dictated in part by the Spetzler-Martin grade. In general, the three options available are:
- microsurgical resection
- endovascular occlusion
- radiosurgery
Occasionally, arteriovenous malformations have been known to spontaneously resolve 2, usually in the setting of intracranial haemorrhage, resulting presumably in venous compression and thrombosis. The annual risk of haemorrhage for an untreated arteriovenous malformation is 2-3%, resulting from a flow-related aneurysm, intra-nidal aneurysm, or venous thrombosis (rarely).
Following haemorrhage, the risk of a further bleed in the next 12 months is up to 18% 5.
Differential diagnosis
Imaging differential considerations include:
- other cerebral vascular malformations
-
cerebral proliferative angiopathy 6,9
- absence of early venous drainage
- often, an entire lobe or even hemisphere is affected
- feeder arteries tend to be of normal size or moderately enlarged
- associated stenosis of feeder arteries is often present
-
craniofacial arteriovenous metameric syndrome (CAMS):
- classic locations
- association with facial AVM
- dural arteriovenous fistula (DAVF)
- developmental venous anomaly (DVA)
-
cerebral proliferative angiopathy 6,9
- vascular tumour
- glioblastoma
-<p><strong>Brain arteriovenous malformations</strong> are type of intracranial high-flow <a href="/articles/cerebrovascular-malformations">vascular malformation</a> composed of enlarged feeding arteries, a nidus of vessels closely associated with the brain parenchyma through which arteriovenous shunting occurs, and draining veins.</p><h4>Terminology</h4><p>This article corresponds to the classic form of arteriovenous malformation involving the brain parenchyma. The term brain arteriovenous malformation (BAVM) is the preferred term <sup>12</sup>. An alternative is <strong>cerebral arteriovenous malformation (CAVM</strong><strong>)</strong>, but the term cerebral leaves out more caudal brain structures and the abbreviation could be confused with <a title="Cavernous malformation" href="/articles/cavernous-venous-malformation-1">cavernous malformation</a>. It is also referred to as a <strong>pial arteriovenous malformation</strong> if it is related to the pial vessels, but this is not always the case <sup>6</sup>.</p><p>These malformations are characterised by a nidus forming the transition between the feeding artery and draining vein. If this transition is made directly, then it is considered an arteriovenous fistula, which is a separate type of cerebral vascular anomaly.</p><h4>Epidemiology</h4><p>Although arteriovenous malformations are thought to represent a congenital abnormality, they are rarely found incidentally in the very young and are thought to expand over time. Despite this, a third of arteriovenous malformations that are diagnosed due to haemorrhage are identified before the age of 20 years <sup>7</sup>. Overall, they are diagnosed at a mean age of 31 years <sup>8</sup>.</p><p>Arteriovenous malformations are thought to occur in approximately 4% of the population but become symptomatic in only 12% of affected individuals <sup>8</sup>. There is no gender predilection <sup>8</sup>.</p><p>AVMs tend to be solitary in the vast majority of cases (>95%). When multiple, syndromic associations must be considered, including:</p><ul>- +<p><strong>Brain arteriovenous malformations</strong> are type of intracranial high-flow <a href="/articles/cerebrovascular-malformations">vascular malformation</a> composed of enlarged feeding arteries, a nidus of vessels closely associated with the brain parenchyma through which arteriovenous shunting occurs, and draining veins.</p><h4>Terminology</h4><p>This article corresponds to the classic form of arteriovenous malformation involving the brain parenchyma. The term brain arteriovenous malformation (BAVM) is the preferred term <sup>12</sup>. An alternative is <strong>cerebral arteriovenous malformation (CAVM</strong><strong>)</strong>, but the term cerebral leaves out more caudal brain structures and the abbreviation could be confused with <a href="/articles/cavernous-venous-malformation-1">cavernous malformation</a>. It is also referred to as a <strong>pial arteriovenous malformation</strong> if it is related to the pial vessels, but this is not always the case <sup>6</sup>.</p><p>These malformations are characterised by a nidus forming the transition between the feeding artery and draining vein. If this transition is made directly, then it is considered an arteriovenous fistula, which is a separate type of cerebral vascular anomaly.</p><h4>Epidemiology</h4><p>Although arteriovenous malformations are thought to represent a congenital abnormality, they are rarely found incidentally in the very young and are thought to expand over time. Despite this, a third of arteriovenous malformations that are diagnosed due to haemorrhage are identified before the age of 20 years <sup>7</sup>. Overall, they are diagnosed at a mean age of 31 years <sup>8</sup>.</p><p>Arteriovenous malformations are thought to occur in approximately 4% of the population but become symptomatic in only 12% of affected individuals <sup>8</sup>. There is no gender predilection <sup>8</sup>.</p><p>AVMs tend to be solitary in the vast majority of cases (>95%). When multiple, syndromic associations must be considered, including:</p><ul>
-<li>other <a href="/articles/cerebral-vascular-malformations">cerebral vascular malformations</a><ul>- +<li>other <a href="/articles/cerebrovascular-malformations">cerebral vascular malformations</a><ul>
-<li><a href="/articles/glioblastoma">glioblastoma</a></li>- +<li><a href="/articles/glioblastoma-idh-wildtype">glioblastoma</a></li>
Image 4 MRI (T2) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.