Chondrosarcoma of the skull base
Updates to Article Attributes
Chondrosarcomas of the base of skull are rare compared with other base of skull tumours, but are an important differential diagnosis as surgical resection and management are affected by the preoperative diagnosis.
Epidemiology
Chondrosarcomas of the base of skull make up only a small fraction of all chondrosarcomas (head and neck chondrosarcomas in one series making up only 7%). They are an even smaller proportion of intracranial neoplasms (making up only ~ 0.2% of all intracranial neoplasms in one series).
Predisposing factors
The vast majority of chondrosarcomas of the base of skull are sporadic, however some predisposing conditions are reported, and include:
- previous trauma / fractures
- Ollier disease
- Maffucci syndrome
Clinical presentation
Patients usually present due to mass effect, either on adjacent brain, brainstem, cranial nerves or (if extension inferiorly) structures of the superior neck.
Pathology
They are thought to arise from embryonal rest cells (remember that the base of skull forms via enchondral ossification).
Location
- petro-occipital synchondrosis (most common)
- sphenoethmoidal junction
- sella turcica
- other rare sites that have been reported (presumably from metaplasia) include:
The majority of chondrosarcomas of the base of skull are located off the midline (82% in one series) a helpful sign compared to chordomas which are usually midline.
Local extension is common, extending intracranially, into the cavernous sinuses, paranasal sinuses and soft tissues beneath the base of skull.
Radiographic features
Chondrosarcomas of the base of skull follow the same general imaging characteristics of chondrosarcomas elsewhere. (see generic chondrosarcoma article)
As a historical note, skull x-rays were important in the diagnosis of these lesions, and demonstrated lytic lesions in 50% and calcifications in approximately 60%. The differentiation of chondrosarcomas from other skull base tumours was very difficult prior to cross-sectional imaging.
MRI protocol
Useful sequences include :
-
T2:
- highhigh signal -
GE:
- calcificationscalcifications typically in rings and arcs -
T1 C+
- usually heterogeneous enhancement
- fat saturation should be employed to better
delineate inferiordelineate inferior component
Treatment and prognosis
They are relatively slow growing but locally aggressive. Metastatic disease is uncommon. Local resection is often the treatment of choice. Radiotherapy may sometimes be employed although sensitivity is thought to be minimal.
Differential diagnosis
Imaging differential considerations include :
- chordoma: usually midline
- meningioma: usually not high T2 signal
- metastases: calcification not as common
-
nasopharyngeal carcinoma (NPC)
- calcification uncommon
- epicentre in nasopharynx
-
pituitary macroadenoma
- calcification uncommon
- centered on pituitary fossa
-<li><a href="/articles/ollier-disease">Ollier disease</a></li>-<li><a href="/articles/maffucci_syndrome">Maffucci syndrome</a></li>- +<li><a href="/articles/enchondromatosis">Ollier disease</a></li>
- +<li><a href="/articles/maffucci-syndrome">Maffucci syndrome</a></li>
-<strong>T2 </strong>- high signal</li>- +<strong>T2:</strong> high signal</li>
-<strong>GE</strong> - calcifications typically in rings and arcs</li>- +<strong>GE:</strong> calcifications typically in rings and arcs</li>
-<li>fat saturation should be employed to better delineate inferior component</li>- +<li>fat saturation should be employed to better delineate inferior component</li>
Image 5 MRI (T1 C+) ( update )

Image 6 MRI (T1 C+) ( update )
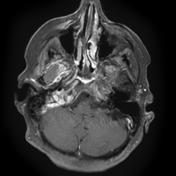
Image 7 MRI (T1 C+) ( create )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.