Creutzfeldt-Jakob disease
Updates to Article Attributes
Creutzfeldt-Jakob disease (CJD) is a spongiform encephalopathy that results in a rapidly progressive dementia and other non-specific neurological features and death usually within a year or less from onset.
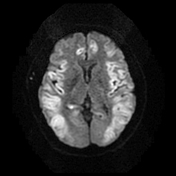
On imaging, it classically manifests as T2/FLAIR hyperintensities within the basal ganglia, the thalamus, and cortex which also show diffusion restriction on DWI/ADC sequences.
Epidemiology
Four types of Creutzfeldt-Jakob disease have been described 2,6:
- sporadic (sCJD): accounts for 85-90% of cases
- variant (vCJD): bovine-to-human transmission of bovine spongiform encephalopathy or mad cow disease (especially if in the UK between 1981-1996), subsequent human-to-human transmission (e.g. transfusion) of vCJD
- familial (fCJD): 10% of cases (these individuals carry a PRPc mutation)
- iatrogenic (iCJD): following administration of cadaveric human pituitary hormones (pre-1985), various transplants
Clinical presentation
Creutzfeldt-Jakob disease is characterised by rapidly progressive dementia, cerebral atrophy, myoclonus, and death. Patients with vCJD present mostly with sensory and psychiatric symptoms; patients with sCJD usually present with progressive cognitive impairment and cerebellar symptoms. Cerebellar symptoms may often be prominent and early in patients with iCJD secondary to cadaveric human pituitary hormones.
Diagnostic markers
- characteristic results on electroencephalography (EEG)
- S100
- CSF 14-3-3 protein: positive result in patient suspected clinically of having sCJD
- CSF and/or olfactory mucosa real time quaking-induced conversion (RT-QuIC) seeding assays: detects minute amounts of the disease-specific pathologic prion protein 12,13
- found to be more
sensitiesensitive than CSF 14-3-3 protein titres 12
- found to be more
A definitive diagnosis requires a brain biopsy, although in many institutions the difficulty involved in sterilising equipment renders a biopsy undesirable.
Pathology
CJD is thought to be mediated via (infectious) prions, a type of protein, which manifests in sheep as the disease scrapie, and in cows as bovine spongiform encephalopathy. Prions are considered infectious in the sense that they can alter the structure of neighbouring proteins.
CJD leads to spongiform degeneration of the brain, which is thought to be caused by the conversion of normal prion protein to proteinaceous infectious particles that accumulate in and around neurons and lead to cell death.
Radiographic features
MRI
MRI findings may be bilateral or unilateral and symmetric or asymmetric, and include:
-
T2: hyperintensity
- basal ganglia (putamen and caudate)
- thalamus (see hockey stick sign and pulvinar sign)
- cortex: most common early manifestation
- white matter
- DWI/ADC: persistent restricted diffusion (considered the most sensitive sign)
Review of sequential studies also typically demonstrates rapidly progressive cerebral atrophy.
Nuclear medicine
- hypometabolism on 18FDG-PET studies
Treatment and prognosis
There is currently no curative treatment and the disease is invariably fatal with a mean survival of only 7 months for most cases.
Since 2009, CJD is a notifiable disease in Australia and by law is required to be reported to the Department of Health. CJD is also notifiable in the United Kingdom, USA and Canada.
History and etymology
It was named after Hans Gerhard Creutzfeldt, a German neurologist who first described the condition in 1920, and Alfons Maria Jakob, a German neurologist who also described the condition in a separate study.
Differential diagnosis
MRI imaging features overlap with many other conditions but the presentation will be different 10,11:
-
autoimmune encephalitis
- particularly anti-D2 dopamine antibodies
- T2 signal change is dominant, with only minor if any diffusion change
- hypoxic/anoxic brain injury
- encephalitis
- hepatic encephalopathy
- hypoglycaemic encephalopathy
- mitochondrial disease
-<li>CSF and/or olfactory mucosa real time quaking-induced conversion (RT-QuIC) seeding assays: detects minute amounts of the disease-specific pathologic prion protein <sup>12,13</sup><ul><li>found to be more sensitie than CSF 14-3-3 protein titres <sup>12</sup>- +<li>CSF and/or olfactory mucosa real time quaking-induced conversion (RT-QuIC) seeding assays: detects minute amounts of the disease-specific pathologic prion protein <sup>12,13</sup><ul><li>found to be more sensitive than CSF 14-3-3 protein titres <sup>12</sup>
Image 15 MRI (DWI) ( create )

Image 16 MRI (DWI) ( create )

Image 17 MRI (DWI) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.