Ewing sarcoma
Updates to Article Attributes
Ewing sarcoma is the second most common highly malignant primary bone tumour of childhood after osteosarcoma, typically arising from medullary cavity with invasion of Haversian system. They usually present as moth-eaten destructive permeative lucent lesions in the shaft of long bones with large soft tissue component without osteoid matrix, and typical onion skin periostitis. It may also involve flat bones and appears sclerotic in up to 30% of cases.
Epidemiology
Typically occurs in children and adolescents between 10 and 20 years of age (95% between 4 and 25 years of age), and has a slight male predilection (M:F 1.5:1) 1-2. It's rare in black people.
Clinical presentation
Presentation is non-specific with local pain being by far the most common symptom. Occasionally a soft tissue mass may be palpable. Pathological fractures also occur. Systemic symptoms including fever may be present. ESR is also elevated.
Pathology
Ewing sarcoma is a small round blue cell tumour with regular sized primitive appearing cells. It is closely related to the soft tissue tumours pPNET, Askin tumour and neuroepithelioma, which collectively are referred to as Ewing sarcoma family of tumours (ESFT) 1. They share not only microscopic appearances but also demonstrate a non-random t(11;22)(q24;q12) chromosome rearrangement.
Location
- lower limb: 45%
- femur most common
- pelvis: 20%
- upper limb: 13%
- spine and ribs: 13%
- sacrococcygeal region most common 4
- skull/face: 2%
Alternatively 3:
- long bones: 50-60%
- femur: 25%
- tibia: 11%
- humerus: 10%
- flat bones: 40%
- pelvis: 14%
- scapula
- ribs: 6%
As far as location within long bones, the tumor is almost always metadiaphyseal or diaphyseal 2-3:
- mid-diaphysis: 33%
- metadiaphysis: 44%
- metaphysis: 15%
- epiphysis: 1-2%
Radiographic features
Ewing sarcomas tend to be large with poorly marginated tumours, with over 80% demonstrating extension into adjacent soft tissues. It should be noted that pPNET often extend into bone, making the distinction difficult.
Plain radiograph and CT
The appearance of these tumours is very variable, but they usually have clearly aggressive appearance. Common findings include 2:
- permeative: 76%
- laminated (onion skin) periosteal reaction: 57%
- sclerosis: 40%
They occasionally demonstrate other appearances, including Codman triangles, spiculated (sunburst) or thick periosteal reaction and even bone expansion or cystic components.
Soft tissue calcification is uncommon, seen in less than 10% of cases 2.
MRI
- T1: low to intermediate signal
- T1 C+ (Gd): heterogeneous but prominent enhancement
- T2: heterogeneously high signal, may see hair on end low signal striations
Nuclear medicine
Ewing sarcomas demonstrate increased uptake on both Gallium67-citrate and all three phases of the Technetium99m methylene diphosphonate bone scans 6.
Treatment and prognosis
Systemic chemotherapy is the mainstay of treatment with surgery and/or radiotherapy playing a role depending of the location and size of the tumour.
What was once a uniformly fatal tumour now has respectable survival rates, although these vary with location. Spinal tumours for example have up to 86% long term survival compared to 25% of sacrococcygeal tumours 4. The overall 5 year survival is in the order of 50-75% of patients with local disease only at the time of presentation 5.
Prognosis is significantly impacted by the presence of distant metastases at the time of diagnosis, which are far more common for the pelvis (25-30%) compared to extremities (<10%) 5. Metastases most frequently go to bone or lungs.
History and etymology
It is named after James Stephen Ewing, American pathologist (1866-1943) 8.
Differential diagnosis
- other Ewing sarcoma family of tumours
- pPNET: large soft tissue component with extension into bone
- Askin tumour: chest wall
- osteosarcoma (ALP is not elevated in Ewing sarcoma)
- osteomyelitis
- metastatic disease
- haematological malignancy
-<p><strong>Ewing sarcoma</strong> is the second most common highly malignant primary bone tumour of childhood after <a href="/articles/osteosarcoma">osteosarcoma</a>, typically arising from medullary cavity with invasion of Haversian system. They usually present as moth-eaten destructive permeative lucent lesions in the shaft of long bones with large soft tissue component without osteoid matrix, and typical onion skin periostitis. It may also involve flat bones and appears sclerotic in up to 30% of cases.</p><h4>Epidemiology</h4><p>Typically occurs in children and adolescents between 10 and 20 years of age (95% between 4 and 25 years of age), and has a slight male predilection (M:F 1.5:1) <sup>1-2</sup>. It's rare in black people.</p><h4>Clinical presentation</h4><p>Presentation is non-specific with local pain being by far the most common symptom. Occasionally a soft tissue mass may be palpable. Pathological fractures also occur. Systemic symptoms including fever may be present. ESR is also elevated.</p><h4>Pathology</h4><p>Ewing sarcoma is a <a href="/articles/small-round-blue-cell-tumours">small round blue cell tumour </a>with regular sized primitive appearing cells. It is closely related to the soft tissue tumours <a href="/articles/ppnet">pPNET</a>, <a href="/articles/askin-tumour-1">Askin tumour</a> and <a href="/articles/neuroepithelioma">neuroepithelioma</a>, which collectively are referred to as <a href="/articles/ewing-sarcoma-family-of-tumours">Ewing sarcoma family of tumours</a> (ESFT) <sup>1</sup>. They share not only microscopic appearances but also demonstrate a non-random t(11;22)(q24;q12) chromosome rearrangement. </p><h5>Location</h5><ul>-<li>lower limb: 45%<ul><li>femur most common</li></ul>-</li>-<li>pelvis: 20%</li>-<li>upper limb: 13%</li>-<li>spine and ribs: 13%<ul><li>sacrococcygeal region most common <sup>4</sup>-</li></ul>-</li>-<li>skull/face: 2%</li>-</ul><p>Alternatively <sup>3</sup>:</p><ul>-<li>long bones: 50-60%<ul>-<li>femur: 25%</li>-<li>tibia: 11%</li>-<li>humerus: 10%</li>-</ul>-</li>-<li>flat bones: 40%<ul>-<li>pelvis: 14%</li>-<li>scapula</li>-<li>ribs: 6%</li>-</ul>-</li>-</ul><p>As far as location within long bones, the tumor is almost always metadiaphyseal or diaphyseal <sup>2-3</sup>:</p><ul>-<li>mid-diaphysis: 33%</li>-<li>metadiaphysis: 44%</li>-<li>metaphysis: 15%</li>-<li>epiphysis: 1-2%</li>-</ul><h4>Radiographic features</h4><p>Ewing sarcomas tend to be large with poorly marginated tumours, with over 80% demonstrating extension into adjacent soft tissues. It should be noted that pPNET often extend into bone, making the distinction difficult.</p><h5>Plain radiograph and CT</h5><p>The appearance of these tumours is very variable, but they usually have clearly aggressive appearance. Common findings include <sup>2</sup>:</p><ul>-<li>-<a href="/articles/permeative-process-in-bone">permeative</a>: 76%</li>-<li>-<a href="/articles/multilayered-periosteal-reaction">laminated (onion skin) periosteal reaction</a>: 57%</li>-<li>sclerosis: 40%</li>-</ul><p>They occasionally demonstrate other appearances, including <a href="/articles/codman-triangle-periosteal-reaction">Codman triangles</a>, spiculated (<a href="/articles/sunburst-appearance-bone-1">sunburst</a>) or thick periosteal reaction and even bone expansion or cystic components.</p><p>Soft tissue calcification is uncommon, seen in less than 10% of cases <sup>2</sup>.</p><h5>MRI</h5><ul>-<li>-<strong>T1:</strong> low to intermediate signal</li>-<li>-<strong>T1 C+ (Gd):</strong> heterogeneous but prominent enhancement</li>-<li>-<strong>T2:</strong> heterogeneously high signal, may see hair on end low signal striations</li>-</ul><h5>Nuclear medicine</h5><p>Ewing sarcomas demonstrate increased uptake on both Gallium<sup>67</sup>-citrate and all three phases of the Technetium<sup>99</sup>m methylene diphosphonate bone scans <sup>6</sup>.</p><h4>Treatment and prognosis</h4><p>Systemic chemotherapy is the mainstay of treatment with surgery and/or radiotherapy playing a role depending of the location and size of the tumour.</p><p>What was once a uniformly fatal tumour now has respectable survival rates, although these vary with location. Spinal tumours for example have up to 86% long term survival compared to 25% of sacrococcygeal tumours <sup>4</sup>. The overall 5 year survival is in the order of 50-75% of patients with local disease only at the time of presentation <sup>5</sup>.</p><p>Prognosis is significantly impacted by the presence of distant metastases at the time of diagnosis, which are far more common for the pelvis (25-30%) compared to extremities (<10%) <sup>5</sup>. Metastases most frequently go to bone or lungs.</p><h4>History and etymology</h4><p>It is named after <strong>James Stephen Ewing</strong>, American pathologist (1866-1943) <sup>8</sup>.</p><h4>Differential diagnosis</h4><ul>-<li>other <a href="/articles/ewing-sarcoma-family-of-tumours">Ewing sarcoma family of tumours</a><ul>-<li>-<a href="/articles/ppnet">pPNET</a>: large soft tissue component with extension into bone</li>-<li>-<a href="/articles/askin-tumour-1">Askin tumour</a>: chest wall</li>-</ul>-</li>-<li>-<a href="/articles/osteosarcoma">osteosarcoma</a> (ALP is not elevated in Ewing sarcoma)</li>-<li><a href="/articles/osteomyelitis">osteomyelitis</a></li>-<li>metastatic disease</li>-<li>haematological malignancy</li>- +<p><strong>Ewing sarcoma</strong> is the second most common highly malignant primary bone tumour of childhood after <a href="/articles/osteosarcoma">osteosarcoma</a>, typically arising from medullary cavity with invasion of Haversian system. They usually present as moth-eaten destructive permeative lucent lesions in the shaft of long bones with large soft tissue component without osteoid matrix, and typical onion skin periostitis. It may also involve flat bones and appears sclerotic in up to 30% of cases.</p><h4>Epidemiology</h4><p>Typically occurs in children and adolescents between 10 and 20 years of age (95% between 4 and 25 years of age), and has a slight male predilection (M:F 1.5:1) <sup>1-2</sup>. It's rare in black people.</p><h4>Clinical presentation</h4><p>Presentation is non-specific with local pain being by far the most common symptom. Occasionally a soft tissue mass may be palpable. Pathological fractures also occur. Systemic symptoms including fever may be present. ESR is also elevated.</p><h4>Pathology</h4><p>Ewing sarcoma is a <a href="/articles/small-round-blue-cell-tumours">small round blue cell tumour </a>with regular sized primitive appearing cells. It is closely related to the soft tissue tumours <a href="/articles/ppnet">pPNET</a>, <a href="/articles/askin-tumour-1">Askin tumour</a> and <a href="/articles/neuroepithelioma">neuroepithelioma</a>, which collectively are referred to as <a href="/articles/ewing-sarcoma-family-of-tumours">Ewing sarcoma family of tumours</a> (ESFT) <sup>1</sup>. They share not only microscopic appearances but also demonstrate a non-random t(11;22)(q24;q12) chromosome rearrangement. </p><h5>Location</h5><ul>
- +<li>lower limb: 45%<ul><li>femur most common</li></ul>
- +</li>
- +<li>pelvis: 20%</li>
- +<li>upper limb: 13%</li>
- +<li>spine and ribs: 13%<ul><li>sacrococcygeal region most common <sup>4</sup>
- +</li></ul>
- +</li>
- +<li>skull/face: 2%</li>
- +</ul><p>Alternatively <sup>3</sup>:</p><ul>
- +<li>long bones: 50-60%<ul>
- +<li>femur: 25%</li>
- +<li>tibia: 11%</li>
- +<li>humerus: 10%</li>
- +</ul>
- +</li>
- +<li>flat bones: 40%<ul>
- +<li>pelvis: 14%</li>
- +<li>scapula</li>
- +<li>ribs: 6%</li>
- +</ul>
- +</li>
- +</ul><p>As far as location within long bones, the tumor is almost always metadiaphyseal or diaphyseal <sup>2-3</sup>:</p><ul>
- +<li>mid-diaphysis: 33%</li>
- +<li>metadiaphysis: 44%</li>
- +<li>metaphysis: 15%</li>
- +<li>epiphysis: 1-2%</li>
- +</ul><h4>Radiographic features</h4><p>Ewing sarcomas tend to be large with poorly marginated tumours, with over 80% demonstrating extension into adjacent soft tissues. It should be noted that pPNET often extend into bone, making the distinction difficult.</p><h5>Plain radiograph and CT</h5><p>The appearance of these tumours is very variable, but they usually have clearly aggressive appearance. Common findings include <sup>2</sup>:</p><ul>
- +<li>
- +<a href="/articles/permeative-process-in-bone">permeative</a>: 76%</li>
- +<li>
- +<a href="/articles/multilayered-periosteal-reaction">laminated (onion skin) periosteal reaction</a>: 57%</li>
- +<li>sclerosis: 40%</li>
- +</ul><p>They occasionally demonstrate other appearances, including <a href="/articles/codman-triangle-periosteal-reaction">Codman triangles</a>, spiculated (<a href="/articles/sunburst-appearance-bone-1">sunburst</a>) or thick periosteal reaction and even bone expansion or cystic components.</p><p>Soft tissue calcification is uncommon, seen in less than 10% of cases <sup>2</sup>.</p><h5>MRI</h5><ul>
- +<li>
- +<strong>T1:</strong> low to intermediate signal</li>
- +<li>
- +<strong>T1 C+ (Gd):</strong> heterogeneous but prominent enhancement</li>
- +<li>
- +<strong>T2:</strong> heterogeneously high signal, may see hair on end low signal striations</li>
- +</ul><h5>Nuclear medicine</h5><p>Ewing sarcomas demonstrate increased uptake on both Gallium<sup>67</sup>-citrate and all three phases of the Technetium<sup>99</sup>m methylene diphosphonate bone scans <sup>6</sup>.</p><h4>Treatment and prognosis</h4><p>Systemic chemotherapy is the mainstay of treatment with surgery and/or radiotherapy playing a role depending of the location and size of the tumour.</p><p>What was once a uniformly fatal tumour now has respectable survival rates, although these vary with location. Spinal tumours for example have up to 86% long term survival compared to 25% of sacrococcygeal tumours <sup>4</sup>. The overall 5 year survival is in the order of 50-75% of patients with local disease only at the time of presentation <sup>5</sup>.</p><p>Prognosis is significantly impacted by the presence of distant metastases at the time of diagnosis, which are far more common for the pelvis (25-30%) compared to extremities (<10%) <sup>5</sup>. Metastases most frequently go to bone or lungs.</p><h4>History and etymology</h4><p>It is named after <strong>James Stephen Ewing</strong>, American pathologist (1866-1943) <sup>8</sup>.</p><h4>Differential diagnosis</h4><ul>
- +<li>other <a href="/articles/ewing-sarcoma-family-of-tumours">Ewing sarcoma family of tumours</a><ul>
- +<li>
- +<a href="/articles/ppnet">pPNET</a>: large soft tissue component with extension into bone</li>
- +<li>
- +<a href="/articles/askin-tumour-1">Askin tumour</a>: chest wall</li>
- +</ul>
- +</li>
- +<li>
- +<a href="/articles/osteosarcoma">osteosarcoma</a> (ALP is not elevated in Ewing sarcoma)</li>
- +<li><a href="/articles/osteomyelitis">osteomyelitis</a></li>
- +<li>metastatic disease</li>
- +<li>haematological malignancy</li>
Image ( destroy )
Image 8 X-ray (Frontal) ( update )

Image 9 MRI (T2 fat sat) ( update )
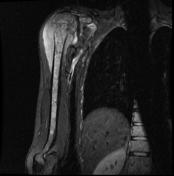
Image 10 CT (bone window) ( update )

Image 11 X-ray (Lateral) ( update )

Image 12 X-ray (Frontal) ( update )

Image 13 X-ray (Frontal and lateral chest radiographs) ( update )

Image 14 X-ray (Frontal) ( update )

Image 15 MRI (T1 C+ fat sat) ( update )

Image 16 MRI (T1) ( update )

Image 17 X-ray (Lateral) ( update )

Image 18 X-ray ( update )

Image 19 CT (bone window) ( update )

Image 20 MRI (STIR) ( update )

Image 21 Nuclear medicine (Coronal) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.