Fetal dosimetry
Updates to Article Attributes
NB - Please consult original article(s) and discuss with you local radiology department / radiation physicist before making any clinical decision.
Although exposure to the gravid uterus is to be avoided when ever possible, and only deliberately performed after careful weighing up of the pros and cons, McCollough et al conclude their recent Radiographics article with: "After comparing the doses from radiologic and nuclear medicine examinations with risk data from human in utero exposures, we have concluded that the absolute risks of fetal effects, including childhood cancer induction, are small at conceptus doses of 100 mGy and negligible at doses of less than 50mGy." 2
Similarly the ACR concluded in 2005 3 “The risk (of abnormality) is considered to be negligible at 50 mGy or less when compared to other risks of pregnancy, and the risk of malformations is significantly increased above control levels only at doses above 150 mGy. Therefore, exposure of the fetus to radiation arising from diagnostic procedures would very rarely be cause, by itself, for terminating a pregnancy.”
Exposure can either be direct (i.e. the fetus is in the field of view) or indirect. When direct the exposure is from both scatter and the primary beam, and typically results in the highest foetal dose. Indirect exposure, when the foetus is not in the field of view, results from scatter from the maternal tissues.
Continuing a pregnancy after radiation exposure? 1
- gestational age < 2 weeks
- < 50 mGy - recommended
- 50 - 150 mGy - recommended
- > 150 mGy - recommended
- gestational age 2 - 8 weeks
- < 50 mGy - recommended
- 50 - 150 mGy - maybe consider termination if other severe risk factors
- > 150 mGy - maybe consider termination if other severe risk factors
- gestational age 8 - 15 weeks
- < 50 mGy - recommended
- 50 - 150 mGy - maybe consider termination if other severe risk factors
- > 150 mGy - higher risk conditions exist but termination is not necessarily recommended
- gestational age 15 weeks to term
- < 50 mGy - recommended
- 50 - 150 mGy - recommended
- > 150 mGy - recommended
Absorbed doses (mGy) to uterus by procedure. 1,2
- cervical spine radiography (AP, lat) : < 0.001
- extremities : < 0.001
- chest x ray (AP,lat) : 0.002
- lumbar spine radiography (AP, lat) : 1 - 4
- pelvic radiography : 2
- hip and femur radiography : 3
- KUB radiography : 2.5
- CT head : ~ 0
- CT chest (including CTPA) : 0.16 - 0.2
- CT upper abdomen : 4
- CT abdomen / pelvis : 30
- CT KUB : 10
-<p><strong>NB - Please consult original article(s) and discuss with you local radiology department / radiation physicist before making any clinical decision.</strong> </p><p>Although exposure to the gravid uterus is to be avoided when ever possible, and only deliberately performed after careful weighing up of the pros and cons, McCollough et al conclude their recent Radiographics article with: "After comparing the doses from radiologic and nuclear medicine examinations with risk data from human in utero exposures, we have concluded that the absolute risks of fetal effects, including childhood cancer induction, are small at conceptus doses of 100 mGy and negligible at doses of less than 50mGy." <sup>2</sup></p><p>Similarly the ACR concluded in 2005 <sup>3</sup> “The risk (of abnormality) is considered to be negligible at 50 mGy or less when compared to other risks of pregnancy, and the risk of malformations is significantly increased above control levels only at doses above 150 mGy. Therefore, exposure of the fetus to radiation arising from diagnostic procedures would very rarely be cause, by itself, for terminating a pregnancy.” </p><p>Exposure can either be direct (i.e. the fetus is in the field of view) or indirect. When direct the exposure is from both scatter and the primary beam, and typically results in the highest foetal dose. Indirect exposure, when the foetus is not in the field of view, results from scatter from the maternal tissues. </p><p>Continuing a pregnancy after radiation exposure? <sup>1</sup> </p><ul>- +<p><strong>NB - Please consult original article(s) and discuss with you local radiology department / radiation physicist before making any clinical decision.</strong></p><p>Although exposure to the gravid uterus is to be avoided when ever possible, and only deliberately performed after careful weighing up of the pros and cons, McCollough et al conclude their recent Radiographics article with: "After comparing the doses from radiologic and nuclear medicine examinations with risk data from human in utero exposures, we have concluded that the absolute risks of fetal effects, including childhood cancer induction, are small at conceptus doses of 100 mGy and negligible at doses of less than 50mGy." <sup>2</sup></p><p>Similarly the ACR concluded in 2005 <sup>3</sup> “The risk (of abnormality) is considered to be negligible at 50 mGy or less when compared to other risks of pregnancy, and the risk of malformations is significantly increased above control levels only at doses above 150 mGy. Therefore, exposure of the fetus to radiation arising from diagnostic procedures would very rarely be cause, by itself, for terminating a pregnancy.”</p><p>Exposure can either be direct (i.e. the fetus is in the field of view) or indirect. When direct the exposure is from both scatter and the primary beam, and typically results in the highest foetal dose. Indirect exposure, when the foetus is not in the field of view, results from scatter from the maternal tissues.</p><p>Continuing a pregnancy after radiation exposure? <sup>1</sup> </p><ul>
-<li>< 50 mGy - recommended </li>-<li>50 - 150 mGy - recommended </li>-<li>> 150 mGy - recommended </li>- +<li>< 50 mGy - recommended</li>
- +<li>50 - 150 mGy - recommended</li>
- +<li>> 150 mGy - recommended</li>
-</li>- +</li>
-<li>< 50 mGy - recommended </li>-<li>50 - 150 mGy - maybe consider termination if other severe risk factors</li>-<li>> 150 mGy - maybe consider termination if other severe risk factors</li>- +<li>< 50 mGy - recommended</li>
- +<li>50 - 150 mGy - maybe consider termination if other severe risk factors</li>
- +<li>> 150 mGy - maybe consider termination if other severe risk factors</li>
-</li>- +</li>
-<li>< 50 mGy - recommended </li>-<li>50 - 150 mGy - maybe consider termination if other severe risk factors</li>-<li>> 150 mGy - higher risk conditions exist but termination is not necessarily recommended </li>- +<li>< 50 mGy - recommended</li>
- +<li>50 - 150 mGy - maybe consider termination if other severe risk factors</li>
- +<li>> 150 mGy - higher risk conditions exist but termination is not necessarily recommended</li>
-</li>- +</li>
-<li>< 50 mGy - recommended </li>-<li>50 - 150 mGy - recommended </li>-<li>> 150 mGy - recommended </li>- +<li>< 50 mGy - recommended</li>
- +<li>50 - 150 mGy - recommended</li>
- +<li>> 150 mGy - recommended</li>
-</li>- +</li>
-<li>cervical spine radiography (AP, lat) : < 0.001</li>-<li>extremities : < 0.001</li>-<li>chest x ray (AP,lat) : 0.002</li>-<li>lumbar spine radiography (AP, lat) : 1 - 4</li>-<li>pelvic radiography : 2</li>-<li>hip and femur radiography : 3</li>-<li>KUB radiography : 2.5 </li>-<li>CT head : ~ 0</li>-<li>CT chest (including CTPA) : 0.16 - 0.2 </li>-<li>CT upper abdomen : 4 </li>-<li>CT abdomen / pelvis : 30 </li>-<li>CT KUB : 10 </li>- +<li>cervical spine radiography (AP, lat) : < 0.001</li>
- +<li>extremities : < 0.001</li>
- +<li>chest x ray (AP,lat) : 0.002</li>
- +<li>lumbar spine radiography (AP, lat) : 1 - 4</li>
- +<li>pelvic radiography : 2</li>
- +<li>hip and femur radiography : 3</li>
- +<li>KUB radiography : 2.5</li>
- +<li>CT head : ~ 0</li>
- +<li>CT chest (including CTPA) : 0.16 - 0.2</li>
- +<li>CT upper abdomen : 4</li>
- +<li>CT abdomen / pelvis : 30</li>
- +<li>CT KUB : 10</li>
Image ( update )
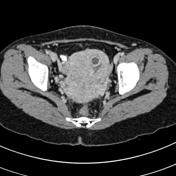
Image 2 CT (C+ portal venous phase) ( update )

Image 3 X-ray (Frontal) ( update )

Image 4 CT (C+ portal venous phase) ( update )

Image 5 CT (C+ portal venous phase) ( update )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.