Medulloblastoma
Updates to Article Attributes
Medulloblastomas are the most common paediatric posterior fossa tumour and account for 30-40% of such entities 7. They are categorised as CNS primitive neuroectodermal tumours (WHO grade IV).
Epidemiology
Medulloblastomas account for 12-25 % of all paediatric CNS tumours, and 30-40% of paediatric posterior fossa tumours 1,7. They are also seen in adults, but only account for 0.4-1.0% of adult brain tumours 1. Since there are many more adults than children, 14-30% of all medulloblastomas are found in adults.
There is a moderate male predilection with a M:F ratio of 2-4:1. They usually present in childhood with 77% of cases before the age of 19. The median age of diagnosis is 9 years. When diagnosed in adulthood, they typically present in the 3rd and 4th decades and are more likely to arise in atypical locations (see below). When they present in adulthood, there is often a better prognosis.
Clinical presentation
Growth of these very cellular tumours is often rapid and accounts for their relatively rapid clinical. Typically, presentation occurs over a few weeks with features that are dominated by symptoms of raised intracranial pressure as a result of obstructive hydrocephalus 7.
In approximately 40% of patients there is evidence of CSF seeding at the time of diagnosis 7.
Pathology
The tumours in general tend to be extremely cellular.
Four 'common' sub types with two additional rare types:
-
classic
- dense sheet like growth of cells
- hyperchromatic round-to-oval nuclei
- increased mitotic activity
- conspicuous apoptosis
- neuroblastic or Homer-Wright rosettes (neoplastic cell nuclei disposed in a radial arrangement around fibrillary processes) are common features
- necrosis is less common
-
desmoplastic
- more common in adults
- once termed "circumscribed arachnoidal cerebellar sarcoma"
- extensively nodular with neuronal differentiation
- usually in children less than 3 years of age
- also known as cerebellar neuroblastoma
- "grapelike" macroscopic nodularity
- intranodular:
- cellular uniformity
- fine fibrillary matrix
- occasional mature ganglion cells
- large cell
- medullomyoblastoma
- melanotic medulloblastoma
Associations
Medullobastomas are associated with a number of syndromes, including:
- Coffin-Siris syndrome
- Cowden syndrome
- Gardner syndrome
- Gorlin syndrome
- Li-Fraumeni syndrome
- Rubinstein-Taybi syndrome
- Turcot syndrome
Radiographic features
The vast majority (94%) of medulloblastomas arise in the cerebellum and the majority of these, from the vermis (75%). They tend to protrude into the fourth ventricle from its roof, and may even grow directly into the brainstem 1,7.
Other areas are uncommon, and are seen more frequent in older children and adults. In such cases the tumour is also more likely to be poorly marginated and demonstrate larger cyst formation 7. Adult medulloblastomas are usually located laterally, in the cerebellar hemispheres, with only 28% centred in the vermis.
Many of its imaging characteristics can be remembered by thinking of medulloblastoma as a small round blue cell tumour. It is also worth remembering that when these tumours are found in an atypical age group (i.e older children or adults) then the appearance and location will be atypical also.
CT
On CT, medulloblastomas appear as a mass arising from the vermis, resulting in effacement of the fourth ventricle / basal cisterns and obstructive hydrocephalus. They are usually hyperdense (90%) and cysts formation / necrosis is common (40 - 50%), especially in older patients. Calcification is seen in 10 - 20% of cases 7.
Enhancement is present in over 90% of cases and is usually prominent 7.
MRI
- T1 - hypointense to grey matter
- T1 C+ (Gd) - 90% enhance, often heterogeneously
-
T2 -
- heterogeneous due to calcification, necrosis and cyst formation
- overall are iso to hyperintense to grey matter
- FLAIR - hyperintense to surrounding brain
- DWI - shows restricted diffusion
- MR spectroscopy - elevated choline, NAA decreased, may show a taurine peak 5
MRI is able to delineate the fourth ventricle and subarachnoid space to a much greater degree than CT. Although medulloblastomas project into the fourth ventricle, unlike ependymomas they do not usually extend into the basal cisterns 7.
As CSF seeding is common at presentation, imaging with contrast of the whole neuraxis is recommended to identify drop metastases and leptomeningeal spread. Although rare, extraneural spread is reported.
Treatment and prognosis
Treatment typically consists of surgical resection, radiation therapy, and chemotherapy. In general the tumours are quite radiosensitive.
Prognosis depends on complete surgical resection, and presence of CSF metastases at the time of diagnosis. Adult onset has a generally better prognosis, as is female gender.
Expression of the c-erbB-2 (HER2/neu) oncogene is useful in staging of medulloblastomas. Increased c-erbB-2 expression reflects an increase in the proliferative activity of a tumour (widely used in breast cancer staging).
- no CSF metastases, complete surgical resection and negative c-erbB-2 expression: 5-year-survival 100%
- no CSF metastases, complete surgical resection and positive c-erbB-2 expression: 5-year-survival 54%
- CSF metastases and/or incomplete surgical resection: 5-year-survival 20%
Differential diagnosis
In the paediatric population consider:
-
ependymoma
- usually arises from the floor of the 4th ventricle
- typically squeezes out the foramen of Luschka
- choroid plexus papilloma (CPP): more common in lateral ventricles in children
- pilocytic astrocytoma
- atypical teratoid / rhabdoid tumour
- brainstem glioma (exophytic)
In the adult population consider:
-<p><strong>Medulloblastomas</strong> are the most common <a href="/articles/posterior-fossa-tumours">paediatric posterior fossa tumour</a> and account for 30-40% of such entities <sup>7</sup>. They are categorised as <a href="/articles/primitive-neuroectodermal-tumour-of-the-cns">CNS primitive neuroectodermal tumours</a> (<a href="/articles/cns-tumours-classification-who">WHO grade IV</a>).</p><h4>Epidemiology</h4><p>Medulloblastomas account for 12-25 % of all paediatric CNS tumours, and 30-40% of paediatric posterior fossa tumours <sup>1,7</sup>. They are also seen in adults, but only account for 0.4-1.0% of <a href="/articles/adult-brain-tumours">adult brain tumours</a> <sup>1</sup>. Since there are many more adults than children, 14-30% of all medulloblastomas are found in adults.</p><p>There is a moderate male predilection with a M:F ratio of 2-4:1. They usually present in childhood with 77% of cases before the age of 19. The median age of diagnosis is 9 years. When diagnosed in adulthood, they typically present in the 3<sup>rd</sup> and 4<sup>th</sup> decades and are more likely to arise in atypical locations (see below). When they present in adulthood, there is often a better prognosis. </p><h4>Clinical presentation</h4><p>Growth of these very cellular tumours is often rapid and accounts for their relatively rapid clinical. Typically, presentation occurs over a few weeks with features that are dominated by symptoms of raised intracranial pressure as a result of <a href="/articles/obstructive_hydrocephalus">obstructive hydrocephalus</a> <sup>7</sup>. </p><p>In approximately 40% of patients there is evidence of CSF seeding at the time of diagnosis <sup>7</sup>.</p><h4>Pathology</h4><p>The tumours in general tend to be extremely cellular.</p><p>Four 'common' sub types with two additional rare types:</p><ol>- +<p><strong>Medulloblastomas</strong> are the most common <a href="/articles/posterior-fossa-tumours">paediatric posterior fossa tumour</a> and account for 30-40% of such entities <sup>7</sup>. They are categorised as <a href="/articles/primitive-neuroectodermal-tumour-of-the-cns">CNS primitive neuroectodermal tumours</a> (<a href="/articles/cns-tumours-classification-who">WHO grade IV</a>).</p><h4>Epidemiology</h4><p>Medulloblastomas account for 12-25 % of all paediatric CNS tumours, and 30-40% of paediatric posterior fossa tumours <sup>1,7</sup>. They are also seen in adults, but only account for 0.4-1.0% of <a href="/articles/adult-brain-tumours">adult brain tumours</a> <sup>1</sup>. Since there are many more adults than children, 14-30% of all medulloblastomas are found in adults.</p><p>There is a moderate male predilection with a M:F ratio of 2-4:1. They usually present in childhood with 77% of cases before the age of 19. The median age of diagnosis is 9 years. When diagnosed in adulthood, they typically present in the 3<sup>rd</sup> and 4<sup>th</sup> decades and are more likely to arise in atypical locations (see below). When they present in adulthood, there is often a better prognosis. </p><h4>Clinical presentation</h4><p>Growth of these very cellular tumours is often rapid and accounts for their relatively rapid clinical. Typically, presentation occurs over a few weeks with features that are dominated by symptoms of raised intracranial pressure as a result of <a href="/articles/obstructive-hydrocephalus">obstructive hydrocephalus</a> <sup>7</sup>. </p><p>In approximately 40% of patients there is evidence of CSF seeding at the time of diagnosis <sup>7</sup>.</p><h4>Pathology</h4><p>The tumours in general tend to be extremely cellular.</p><p>Four 'common' sub types with two additional rare types:</p><ol>
-<li><a href="/articles/gardner_syndrome">Gardner syndrome</a></li>- +<li><a href="/articles/gardner-syndrome">Gardner syndrome</a></li>
-<li><a href="/articles/turcot_syndrome">Turcot syndrome</a></li>- +<li><a href="/articles/turcot-syndrome">Turcot syndrome</a></li>
-<li><a href="/articles/pilocytic_astrocytoma">pilocytic astrocytoma</a></li>- +<li><a href="/articles/pilocytic-astrocytoma">pilocytic astrocytoma</a></li>
Image ( update )
Image 1 Pathology (Gross pathology) ( update )

Image 2 MRI (T2) ( update )
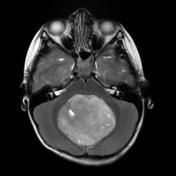
Image 3 CT (non-contrast) ( update )

Image 4 MRI (T1 C+ fat sat) ( update )

Image 5 MRI (T1 C+) ( update )

Image 6 MRI (T1 C+) ( update )

Image 7 MRI (T2) ( create )

Image 12 MRI (ADC) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.