Sickle cell disease
Updates to Article Attributes
Sickle cell disease (SCD) (historically also known as drepanocytosis) is a hereditary (autosomal recessive) condition resulting in the formation of abnormal haemoglobin (a haemoglobinopathy), which manifests as multisystem ischaemia and infarction, as well as haemolytic anaemia.
Haemoglobin SC (HbSC) disease, although a sickle cell disease subtype, with similarities to the classic condition, should ideally be considered as a distinct pathological entity 7.
Terminology
The term sickle cell disease is preferred to sickle cell anaemia for the name of the condition, not least because the former term reflects the fact that the condition has multisystem effects, rather than just a severe form of anaemia.
Epidemiology
There is no recognised gender predilection. The highest incidence occurs in individuals of African descent, followed by eastern Mediterranean and Middle Eastern populations. Malaria is the strongest known selective pressure on the human genome. The sickle cell mutation is prevalent in part as it confers a human genetic resistance to malaria as the abnormal haemoglobin has higher turnover and increased phagocytosis while sickled red cells have reduced cell-cell cytoadherence preventing the parasite from multiplying during the erythrocytic phase of its life cycle. It is estimated that approximately 8% of the African population is homozygous for sickle cell (where malaria is most prevalent).
Clinical presentation
The earliest manifestation is usually in early childhood, as babies are protected by elevated levels of fetal haemoglobin (HbF) in the first 6 months 3. The first presentation is commonly a painful vaso-occlusive crisis: sudden onset of bone or visceral pain due to microvascular occlusion and ischaemia, often in the setting of sepsis or dehydration. Sickle cell disease is known to have a wide spectrum of clinical presentations from completely asymptomatic to a severe overwhelming crisis.
Clinical findings are wide and include 1,6:
- bone pain
- pulmonary
- acute chest syndrome
- recurrent pneumonia (impaired immunity due to functional asplenia)
- chronic lung disease
- abdominal
- abdominal pain from vaso-occlusive crises
- sequestration syndrome (rapid pooling of blood in the spleen leading to intravascular volume depletion)
- haemolytic anaemia and extramedullary haematopoiesis
- impaired immunity from autosplenectomy
- multiple renal manifestations, with end result of renal failure 5
- cerebral
- stroke
- cognitive impairment
- ocular and orbital complications
- priapism
- leg ulcers
Pathology
The disease results from a mutation in a gene coding for the beta chain of the haemoglobin molecule termed HbS. Specifically, there is a substitution of glutamine for valine at the 6th position in the beta-globin chain.
The term "sickle cell disease" applies to all patients who have two abnormal beta chains. The resultant haemoglobin molecules tend to clump together into long polymers, making the red blood cell (RBC) elongated (sickle-shaped), rigid and unable to deform appropriately when passing through small vessels, resulting in vascular occlusion. The abnormal RBCs are also removed from the bloodstream at an increased rate, leading to a haemolytic anaemia 1.
Individuals with one HbS beta chain and one normal beta chain are said to have the "sickle cell trait". They are usually asymptomatic, although there is an association with an increased risk of renal medullary carcinoma 2. Perhaps of some consolation to individuals with the sickle cell trait is the increased resistance to malaria.
Individuals with one HbS beta chain and one haemoglobin C (HbC) beta chain, have a subtype of sickle cell disease known as haemoglobin SC (HbSC) disease 7.
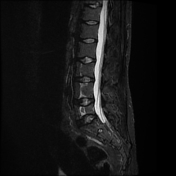
Radiographic features
The radiographic manifestations of sickle cell disease are protean and are best discussed individually. Below is a summary of the main findings with links to individual articles.
Skeletal
Musculoskeletal manifestations of sickle cell disease are discussed separately. Three separate mechanisms can result in skeletal changes 6:
- chronic anaemia resulting in expansion of the medullary spaces
- vaso-occlusive crises resulting in bone infarcts and subperiosteal haemorrhages
- infection
These, in turn, can predispose individuals to other complications, such as growth disturbance and pathological fractures.
Pulmonary
Pulmonary involvement is a leading cause of mortality among sickle cell disease patients and can be acute or chronic:
Cardiovascular
- elevated cardiac output resulting in
- cardiomegaly 9
- left ventricular dysfunction
- diastolic dysfunction
Abdominal
Abdominal manifestations of sickle cell disease are discussed separately. Splenic infarction and subsequent functional asplenia tend to occur early in the disease. The hepatobiliary and renal systems are also commonly involved.
Cerebral
Cerebral manifestations of sickle cell disease are discussed separately. Stroke and cerebral atrophy are common neurologic sequelae of sickle cell disease.
Extramedullary haematopoiesis
Extramedullary haematopoiesis is discussed separately. Less common in sickle cell disease than in other haemolytic anaemias. The most common site is liver, followed by spleen, thorax, and adrenals 4.
Treatment and prognosis
Management of vaso-occlusive crises includes oxygen, hydration, and analgesia. Hydroxyurea decreases the severity of vaso-occlusive crises 1. Anaemia is usually well-tolerated, however, blood transfusions may be indicated in some cases. Bone marrow transplantation may provide a cure.
Sickle cell disease is associated with reduced life expectancy, whereas individuals with sickle cell trait have a normal life expectancy.
See also
-<p><strong>Sickle cell disease (SCD)</strong> (historically also known as drepanocytosis) is a hereditary (autosomal recessive) condition resulting in the formation of abnormal <a href="/articles/haemoglobin">haemoglobin</a> (a <a href="/articles/haemoglobinopathies">haemoglobinopathy</a>), which manifests as multisystem ischaemia and infarction, as well as <a href="/articles/haemolytic-anaemia">haemolytic anaemia</a>. </p><p><a href="/articles/haemoglobin-sc-disease">Haemoglobin SC (HbSC) disease</a>, although a sickle cell disease subtype, with similarities to the classic condition, should ideally be considered as a distinct pathological entity <sup>7</sup>.</p><h4>Terminology</h4><p>The term sickle cell disease is preferred to sickle cell anaemia for the name of the condition, not least because the former term reflects the fact that the condition has multisystem effects, rather than just a severe form of anaemia. </p><h4>Epidemiology</h4><p>There is no recognised gender predilection. The highest incidence occurs in individuals of African descent, followed by eastern Mediterranean and Middle Eastern populations. Malaria is the strongest known selective pressure on the human genome. The sickle cell mutation is prevalent in part as it confers a human genetic resistance to malaria as the abnormal haemoglobin has higher turnover and increased phagocytosis while sickled red cells have reduced cell-cell cytoadherence preventing the parasite from multiplying during the erythrocytic phase of its life cycle. It is estimated that approximately 8% of the African population is homozygous for sickle cell (where malaria is most prevalent).</p><h4>Clinical presentation</h4><p>The earliest manifestation is usually in early childhood, as babies are protected by elevated levels of fetal haemoglobin (HbF) in the first 6 months <sup>3</sup>. The first presentation is commonly a painful vaso-occlusive crisis: sudden onset of bone or visceral pain due to microvascular occlusion and ischaemia, often in the setting of sepsis or dehydration. Sickle cell disease is known to have a wide spectrum of clinical presentations from completely asymptomatic to a severe overwhelming crisis.</p><p>Clinical findings are wide and include <sup>1,6</sup>:</p><ul>-<li>bone pain<ul>-<li><a href="/articles/bone-infarction-1">bone infarction</a></li>-<li><a href="/articles/subperiosteal-haemorrhage">subperiosteal haemorrhage</a></li>-<li><a href="/articles/osteomyelitis">osteomyelitis</a></li>-</ul>-</li>-<li>pulmonary<ul>-<li><a href="/articles/sickle-cell-disease-acute-chest-syndrome-1">acute chest syndrome </a></li>-<li>recurrent <a href="/articles/pneumonia">pneumonia</a> (impaired immunity due to functional asplenia)</li>-<li><a href="/articles/sickle-cell-disease-chronic-lung-disease-1">chronic lung disease </a></li>-</ul>-</li>-<li>abdominal<ul>-<li>abdominal pain from vaso-occlusive crises<ul><li>-<a title="girdle syndrome" href="/articles/girdle-syndrome">girdle syndrome</a> <sup>10</sup>-</li></ul>-</li>-<li>-<a href="/articles/sequestration-syndrome">sequestration syndrome </a>(rapid pooling of blood in the spleen leading to intravascular volume depletion)</li>-</ul>-</li>-<li>-<a href="/articles/haemolytic-anaemia">haemolytic anaemia</a> and <a href="/articles/extramedullary-haematopoiesis">extramedullary haematopoiesis</a>-</li>-<li>impaired immunity from <a href="/articles/autosplenectomy">autosplenectomy</a>-</li>-<li>multiple renal manifestations, with end result of <a href="/articles/end-stage-renal-disease-2">renal failure</a> <sup>5</sup>-</li>-<li>cerebral<ul>-<li><a href="/articles/stroke">stroke</a></li>-<li>cognitive impairment</li>-</ul>-</li>-<li>ocular and orbital complications<ul><li>-<a href="/articles/central-retinal-artery-occlusion">central retinal artery occlusion</a> (CRAO)</li></ul>-</li>-<li><a href="/articles/priapism">priapism</a></li>-<li>leg ulcers</li>-</ul><h4>Pathology</h4><p>The disease results from a mutation in a gene coding for the beta chain of the haemoglobin molecule termed HbS. Specifically, there is a substitution of glutamine for valine at the 6th position in the beta-globin chain.</p><p>The term "sickle cell disease" applies to all patients who have two abnormal beta chains. The resultant haemoglobin molecules tend to clump together into long polymers, making the red blood cell (RBC) elongated (sickle-shaped), rigid and unable to deform appropriately when passing through small vessels, resulting in vascular occlusion. The abnormal RBCs are also removed from the bloodstream at an increased rate, leading to a haemolytic anaemia <sup>1</sup>.</p><p>Individuals with one HbS beta chain and one normal beta chain are said to have the "<a href="/articles/sickle-cell-trait">sickle cell trait</a>". They are usually asymptomatic, although there is an association with an increased risk of <a href="/articles/renal-medullary-carcinoma">renal medullary carcinoma</a> <sup>2</sup>. Perhaps of some consolation to individuals with the sickle cell trait is the increased resistance to malaria.</p><p>Individuals with one HbS beta chain and one haemoglobin C (HbC) beta chain, have a subtype of sickle cell disease known as <a href="/articles/haemoglobin-sc-disease">haemoglobin SC (HbSC) disease</a> <sup>7</sup>. </p><h4>Radiographic features</h4><p>The radiographic manifestations of sickle cell disease are protean and are best discussed individually. Below is a summary of the main findings with links to individual articles. </p><h5>Skeletal</h5><p><a href="/articles/sickle-cell-disease-skeletal-manifestations-1">Musculoskeletal manifestations of sickle cell disease</a> are discussed separately. Three separate mechanisms can result in skeletal changes <sup>6</sup>: </p><ol>-<li>chronic anaemia resulting in expansion of the medullary spaces</li>-<li>vaso-occlusive crises resulting in bone infarcts and subperiosteal haemorrhages</li>-<li>infection</li>-</ol><p>These, in turn, can predispose individuals to other complications, such as growth disturbance and pathological fractures.</p><h5>Pulmonary</h5><p>Pulmonary involvement is a leading cause of mortality among sickle cell disease patients and can be acute or chronic:</p><ul>-<li><a href="/articles/sickle-cell-disease-acute-chest-syndrome-1">acute chest syndrome in sickle cell anaemia</a></li>-<li><a href="/articles/sickle-cell-disease-chronic-lung-disease-1">chronic lung disease in sickle cell anaemia</a></li>-</ul><h5>Cardiovascular</h5><ul><li>elevated cardiac output resulting in <ul>-<li>cardiomegaly<sup> 9</sup>-</li>-<li>left ventricular dysfunction</li>-<li>diastolic dysfunction</li>-</ul>-</li></ul><h5>Abdominal</h5><p><a href="/articles/sickle-cell-disease-abdominal-manifestations-1">Abdominal manifestations of sickle cell disease</a> are discussed separately. <a href="/articles/splenic-infarction">Splenic infarction</a> and subsequent <a href="/articles/asplenia">functional asplenia</a> tend to occur early in the disease. The hepatobiliary and renal systems are also commonly involved.</p><h5>Cerebral</h5><p><a href="/articles/sickle-cell-disease-cerebral-manifestations-1">Cerebral manifestations of sickle cell disease</a> are discussed separately. Stroke and cerebral atrophy are common neurologic sequelae of sickle cell disease.</p><h5>Extramedullary haematopoiesis</h5><p><a href="/articles/extramedullary-haematopoiesis">Extramedullary haematopoiesis</a> is discussed separately. Less common in sickle cell disease than in other haemolytic anaemias. The most common site is liver, followed by spleen, thorax, and adrenals <sup>4</sup>.</p><h4>Treatment and prognosis</h4><p>Management of vaso-occlusive crises includes oxygen, hydration, and analgesia. Hydroxyurea decreases the severity of vaso-occlusive crises <sup>1</sup>. Anaemia is usually well-tolerated, however, blood transfusions may be indicated in some cases. <a href="/articles/haematopoietic-stem-cell-transplantation">Bone marrow transplantation</a> may provide a cure.</p><p>Sickle cell disease is associated with reduced life expectancy, whereas individuals with sickle cell trait have a normal life expectancy.</p><h4>See also</h4><ul>-<li><a href="/articles/osteosclerosis-causes-mnemonic">dense bone mnemonic</a></li>-<li><a href="/articles/thalassemia">thalassaemia</a></li>- +<p><strong>Sickle cell disease (SCD)</strong> (historically also known as drepanocytosis) is a hereditary (autosomal recessive) condition resulting in the formation of abnormal <a href="/articles/haemoglobin">haemoglobin</a> (a <a href="/articles/haemoglobinopathies">haemoglobinopathy</a>), which manifests as multisystem ischaemia and infarction, as well as <a href="/articles/haemolytic-anaemia">haemolytic anaemia</a>. </p><p><a href="/articles/haemoglobin-sc-disease">Haemoglobin SC (HbSC) disease</a>, although a sickle cell disease subtype, with similarities to the classic condition, should ideally be considered as a distinct pathological entity <sup>7</sup>.</p><h4>Terminology</h4><p>The term sickle cell disease is preferred to sickle cell anaemia for the name of the condition, not least because the former term reflects the fact that the condition has multisystem effects, rather than just a severe form of anaemia. </p><h4>Epidemiology</h4><p>There is no recognised gender predilection. The highest incidence occurs in individuals of African descent, followed by eastern Mediterranean and Middle Eastern populations. Malaria is the strongest known selective pressure on the human genome. The sickle cell mutation is prevalent in part as it confers a human genetic resistance to malaria as the abnormal haemoglobin has higher turnover and increased phagocytosis while sickled red cells have reduced cell-cell cytoadherence preventing the parasite from multiplying during the erythrocytic phase of its life cycle. It is estimated that approximately 8% of the African population is homozygous for sickle cell (where malaria is most prevalent).</p><h4>Clinical presentation</h4><p>The earliest manifestation is usually in early childhood, as babies are protected by elevated levels of fetal haemoglobin (HbF) in the first 6 months <sup>3</sup>. The first presentation is commonly a painful vaso-occlusive crisis: sudden onset of bone or visceral pain due to microvascular occlusion and ischaemia, often in the setting of sepsis or dehydration. Sickle cell disease is known to have a wide spectrum of clinical presentations from completely asymptomatic to a severe overwhelming crisis.</p><p>Clinical findings are wide and include <sup>1,6</sup>:</p><ul>
- +<li>bone pain<ul>
- +<li><a href="/articles/bone-infarction-1">bone infarction</a></li>
- +<li><a href="/articles/subperiosteal-haemorrhage">subperiosteal haemorrhage</a></li>
- +<li><a href="/articles/osteomyelitis">osteomyelitis</a></li>
- +</ul>
- +</li>
- +<li>pulmonary<ul>
- +<li><a href="/articles/sickle-cell-disease-acute-chest-syndrome-1">acute chest syndrome </a></li>
- +<li>recurrent <a href="/articles/pneumonia">pneumonia</a> (impaired immunity due to functional asplenia)</li>
- +<li><a href="/articles/sickle-cell-disease-chronic-lung-disease-1">chronic lung disease </a></li>
- +</ul>
- +</li>
- +<li>abdominal<ul>
- +<li>abdominal pain from vaso-occlusive crises<ul><li>
- +<a title="girdle syndrome" href="/articles/girdle-syndrome">girdle syndrome</a> <sup>10</sup>
- +</li></ul>
- +</li>
- +<li>
- +<a href="/articles/sequestration-syndrome">sequestration syndrome </a>(rapid pooling of blood in the spleen leading to intravascular volume depletion)</li>
- +</ul>
- +</li>
- +<li>
- +<a href="/articles/haemolytic-anaemia">haemolytic anaemia</a> and <a href="/articles/extramedullary-haematopoiesis">extramedullary haematopoiesis</a>
- +</li>
- +<li>impaired immunity from <a href="/articles/autosplenectomy">autosplenectomy</a>
- +</li>
- +<li>multiple renal manifestations, with end result of <a href="/articles/end-stage-renal-disease-2">renal failure</a> <sup>5</sup>
- +</li>
- +<li>cerebral<ul>
- +<li><a href="/articles/stroke">stroke</a></li>
- +<li>cognitive impairment</li>
- +</ul>
- +</li>
- +<li>ocular and orbital complications<ul><li>
- +<a href="/articles/central-retinal-artery-occlusion-1">central retinal artery occlusion</a> (CRAO)</li></ul>
- +</li>
- +<li><a href="/articles/priapism">priapism</a></li>
- +<li>leg ulcers</li>
- +</ul><h4>Pathology</h4><p>The disease results from a mutation in a gene coding for the beta chain of the haemoglobin molecule termed HbS. Specifically, there is a substitution of glutamine for valine at the 6th position in the beta-globin chain.</p><p>The term "sickle cell disease" applies to all patients who have two abnormal beta chains. The resultant haemoglobin molecules tend to clump together into long polymers, making the red blood cell (RBC) elongated (sickle-shaped), rigid and unable to deform appropriately when passing through small vessels, resulting in vascular occlusion. The abnormal RBCs are also removed from the bloodstream at an increased rate, leading to a haemolytic anaemia <sup>1</sup>.</p><p>Individuals with one HbS beta chain and one normal beta chain are said to have the "<a href="/articles/sickle-cell-trait">sickle cell trait</a>". They are usually asymptomatic, although there is an association with an increased risk of <a href="/articles/renal-medullary-carcinoma">renal medullary carcinoma</a> <sup>2</sup>. Perhaps of some consolation to individuals with the sickle cell trait is the increased resistance to malaria.</p><p>Individuals with one HbS beta chain and one haemoglobin C (HbC) beta chain, have a subtype of sickle cell disease known as <a href="/articles/haemoglobin-sc-disease">haemoglobin SC (HbSC) disease</a> <sup>7</sup>. </p><h4>Radiographic features</h4><p>The radiographic manifestations of sickle cell disease are protean and are best discussed individually. Below is a summary of the main findings with links to individual articles. </p><h5>Skeletal</h5><p><a href="/articles/sickle-cell-disease-skeletal-manifestations-1">Musculoskeletal manifestations of sickle cell disease</a> are discussed separately. Three separate mechanisms can result in skeletal changes <sup>6</sup>: </p><ol>
- +<li>chronic anaemia resulting in expansion of the medullary spaces</li>
- +<li>vaso-occlusive crises resulting in bone infarcts and subperiosteal haemorrhages</li>
- +<li>infection</li>
- +</ol><p>These, in turn, can predispose individuals to other complications, such as growth disturbance and pathological fractures.</p><h5>Pulmonary</h5><p>Pulmonary involvement is a leading cause of mortality among sickle cell disease patients and can be acute or chronic:</p><ul>
- +<li><a href="/articles/sickle-cell-disease-acute-chest-syndrome-1">acute chest syndrome in sickle cell anaemia</a></li>
- +<li><a href="/articles/sickle-cell-disease-chronic-lung-disease-1">chronic lung disease in sickle cell anaemia</a></li>
- +</ul><h5>Cardiovascular</h5><ul><li>elevated cardiac output resulting in <ul>
- +<li>cardiomegaly<sup> 9</sup>
- +</li>
- +<li>left ventricular dysfunction</li>
- +<li>diastolic dysfunction</li>
- +</ul>
- +</li></ul><h5>Abdominal</h5><p><a href="/articles/sickle-cell-disease-abdominal-manifestations-1">Abdominal manifestations of sickle cell disease</a> are discussed separately. <a href="/articles/splenic-infarction">Splenic infarction</a> and subsequent <a href="/articles/asplenia">functional asplenia</a> tend to occur early in the disease. The hepatobiliary and renal systems are also commonly involved.</p><h5>Cerebral</h5><p><a href="/articles/sickle-cell-disease-cerebral-manifestations-1">Cerebral manifestations of sickle cell disease</a> are discussed separately. Stroke and cerebral atrophy are common neurologic sequelae of sickle cell disease.</p><h5>Extramedullary haematopoiesis</h5><p><a href="/articles/extramedullary-haematopoiesis">Extramedullary haematopoiesis</a> is discussed separately. Less common in sickle cell disease than in other haemolytic anaemias. The most common site is liver, followed by spleen, thorax, and adrenals <sup>4</sup>.</p><h4>Treatment and prognosis</h4><p>Management of vaso-occlusive crises includes oxygen, hydration, and analgesia. Hydroxyurea decreases the severity of vaso-occlusive crises <sup>1</sup>. Anaemia is usually well-tolerated, however, blood transfusions may be indicated in some cases. <a href="/articles/haematopoietic-stem-cell-transplantation">Bone marrow transplantation</a> may provide a cure.</p><p>Sickle cell disease is associated with reduced life expectancy, whereas individuals with sickle cell trait have a normal life expectancy.</p><h4>See also</h4><ul>
- +<li><a href="/articles/osteosclerosis-causes-mnemonic">dense bone mnemonic</a></li>
- +<li><a href="/articles/thalassemia">thalassaemia</a></li>
Image 10 MRI (STIR) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.