Traumatic spinal cord injury
Updates to Article Attributes
Traumatic spinal cord injury (SCI) can manifest as a wide variety of clinical syndromes resulting from damage to the spinal cord or its surrounding structures. It can result from minor injury if the spine is weakened from disease disease such as ankylosing spondylitis or if there is pre-existing spinal stenosis. It is an emergency emergency which can require urgent surgical intervention to prevent long term neurological complications of spinal cord injury.
Clinical presentation
The mechanism of injury varies and can include:
road traffic accidentssports injuriesassault or gunshot injuryfalls
In addition to neurological signs of altered sensation, limb weakness, autonomic dysfunction, and sphincter disruption there is usually pain due to related injury to the musculoskeletal components of the spine.
Recognised neurological syndromes of spinal injury from trauma include:
- anterior cord syndrome
- Brown-Séquard syndrome
- cauda equina syndrome
- central cord syndrome
- conus medullaris syndrome
- spinal cord transection
Pathology
There are several types of traumatic SCI 3,4,5:
- spinal cord swelling
-
spinal cord contusion/oedema
- cord oedema only: most favourable prognosis
- cord oedema and contusion: intermediate prognosis
- cord contusion only: worse prognosis
- intramedullary haemorrhage
- extrinsic compression, e.g. from fracture fragment or disc herniation
- spinal cord transection
Mechanism
The mechanism of injury varies and can include:
- road traffic accidents
- sports injuries
- assault or gunshot injury
- falls
Classification
Injuries can be complete or incomplete at a specified level, which can be classified using. The most common system is the ASIA standardsInternal Standards for spinal cord injuryNeurological Classification of Spinal Cord Injury (ISNCSCI) from the American Spinal Injury Association (ASIA) 2.
Recognised neurological syndromes of spinal injury from trauma include:
cauda equina syndromecentral cord syndromeBrown-Séquard syndromeanterior cord syndromespinal cord transection
Pathology
content pending
Radiographic appearance
RadiographPlain radiograph
These have no real role in traumatic cord injury in patients with significant trauma as they have limited sensitivity for detecting spinal cord trauma and bony bony injuries associated with it.
CT
This is best for assessing the associated bony injuries which may need concomitant treatment consideration, but does not assess the cord itself.
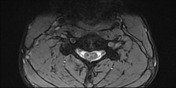
MRI
Apart from routine axial and sagitalsagittal T1 and T2 imaging additional sequences should be considered depending on the clinical concern. T2* sequences (e.g. Gradientgradient echo or , SWI is) are more sensitive for haemorrhage, while STIR sequences are more sensitive for associated ligamentous injury.
-
haemorrhagelow signal on T2 and gradient echo acutely-
seeageing blood on MRIfor other timescales
-
contusionhigh T2 signal above or below level of trauma
-
spinal cord swelling
- focal cord enlargement at level of trauma without signal change 5best seen on
sagitalsagittal T1
- focal cord enlargement at level of trauma without signal change 5best seen on
-
spinal cord oedema
- as per swelling but with additional increased T2 signal
-
spinal cord contusion
- thick high T2 signal rim around small central low T1 signal above or below level of trauma 5
- blooming on T2* sequences
-
intramedullary haemorrhage
- thin high T2 signal rim around large central low T1 signal 5
- blooming on T2* sequences
- see ageing blood on MRI for other timescales
-
spinal cord transection
- discontinuity of cord best seen on sagittal sequences
-<p><strong>Traumatic spinal cord injury </strong>can manifest as a wide variety of clinical syndromes resulting from damage to the spinal cord or its surrounding structures. It can result from minor injury if the spine is weakened from disease such as ankylosing spondylitis or if there is pre-existing spinal stenosis. It is an emergency which can require urgent surgical intervention to prevent long term neurological complications of spinal cord injury.</p><h4>Clinical presentation</h4><p>The mechanism of injury varies and can include:</p><ul>- +<p><strong>Traumatic spinal cord injury (SCI) </strong>can manifest as a wide variety of clinical syndromes resulting from damage to the spinal cord or its surrounding structures. It can result from minor injury if the spine is weakened from disease such as ankylosing spondylitis or if there is pre-existing spinal stenosis. It is an emergency which can require urgent surgical intervention to prevent long term neurological complications of spinal cord injury.</p><h4>Clinical presentation</h4><p>In addition to neurological signs of altered sensation, limb weakness, autonomic dysfunction, and sphincter disruption there is usually pain due to related injury to the musculoskeletal components of the spine.</p><p>Recognised neurological syndromes of spinal injury from trauma include:</p><ul>
- +<li><a href="/articles/anterior-cord-syndrome">anterior cord syndrome</a></li>
- +<li><a href="/articles/brown-sequard-syndrome-1">Brown-Séquard syndrome</a></li>
- +<li><a href="/articles/cauda-equina-syndrome">cauda equina syndrome</a></li>
- +<li><a href="/articles/central-cord-syndrome">central cord syndrome</a></li>
- +<li><a href="/articles/conus-medullaris-syndrome">conus medullaris syndrome</a></li>
- +<li><a href="/articles/spinal-cord-transection">spinal cord transection</a></li>
- +</ul><h4>Pathology</h4><p>There are several types of traumatic SCI <sup>3,4,5</sup>:</p><ul>
- +<li>spinal cord swelling</li>
- +<li>spinal cord contusion/oedema<ul>
- +<li>cord oedema only: most favourable prognosis</li>
- +<li>cord oedema and contusion: intermediate prognosis</li>
- +<li>cord contusion only: worse prognosis</li>
- +</ul>
- +</li>
- +<li>intramedullary haemorrhage</li>
- +<li>extrinsic compression, e.g. from fracture fragment or disc herniation</li>
- +<li><a href="/articles/spinal-cord-transection">spinal cord transection</a></li>
- +</ul><h5>Mechanism</h5><p>The mechanism of injury varies and can include:</p><ul>
-</ul><p>In addition to neurological signs of altered sensation, limb weakness, autonomic dysfunction, and sphincter disruption there is usually pain due to related injury to the musculoskeletal components of the spine. Injuries can be complete or incomplete at a specified level, which can be classified using the ASIA standards for spinal cord injury.</p><p>Recognised neurological syndromes of spinal injury from trauma include:</p><ul>-<li><a href="/articles/cauda-equina-syndrome">cauda equina syndrome</a></li>-<li><a href="/articles/acute-traumatic-central-cord-syndrome">central cord syndrome</a></li>-<li><a href="/articles/brown-sequard-syndrome-1">Brown-Séquard syndrome</a></li>-<li><a href="/articles/anterior-cord-syndrome">anterior cord syndrome</a></li>-<li><a href="/articles/spinal-cord-transection">spinal cord transection</a></li>-</ul><h4>Pathology</h4><ul><li><em>content pending</em></li></ul><h4>Radiographic appearance</h4><h5>Radiograph</h5><p>These have no real role in traumatic cord injury in patients with significant trauma as they have limited sensitivity for detecting spinal cord trauma and bony injuries associated with it.</p><h5>CT</h5><p>This is best for assessing the associated bony injuries which may need concomitant treatment consideration, but does not assess the cord itself.</p><h5>MRI</h5><p>Apart from routine axial and sagital T1 and T2 imaging additional sequences should be considered depending on the clinical concern. <a href="/articles/gradient-echo-sequences-1">Gradient echo</a> or <a href="/articles/susceptibility-weighted-imaging-1">SWI</a> is more sensitive for haemorrhage while STIR sequences are more sensitive for associated ligamentous injury.</p><ul>-<li>haemorrhage<ul>-<li>low signal on T2 and gradient echo acutely</li>-<li>see <a href="/articles/ageing-blood-on-mri">ageing blood on MRI </a>for other timescales</li>- +</ul><h4>Classification</h4><p>Injuries can be complete or incomplete at a specified level. The most common system is the <a href="/articles/internal-standards-for-neurological-classification-of-spinal-cord-injury">Internal Standards for Neurological Classification of Spinal Cord Injury</a> (ISNCSCI) from the American Spinal Injury Association (ASIA) <sup>2</sup>.</p><h4>Radiographic appearance</h4><h5>Plain radiograph</h5><p>These have no real role in traumatic cord injury in patients with significant trauma as they have limited sensitivity for detecting spinal cord trauma and bony injuries associated with it.</p><h5>CT</h5><p>This is best for assessing the associated bony injuries which may need concomitant treatment consideration, but does not assess the cord itself.</p><h5>MRI</h5><p>Apart from routine axial and sagittal T1 and T2 imaging additional sequences should be considered depending on the clinical concern. T2* sequences (e.g. <a href="/articles/gradient-echo-sequences-1">gradient echo</a>, <a href="/articles/susceptibility-weighted-imaging-1">SWI</a>) are more sensitive for haemorrhage, while STIR sequences are more sensitive for associated ligamentous injury.</p><ul>
- +<li>spinal cord swelling<ul><li>focal cord enlargement at level of trauma without signal change <sup>5</sup> best seen on sagittal T1</li></ul>
- +</li>
- +<li>spinal cord oedema<ul><li>as per swelling but with additional increased T2 signal </li></ul>
- +</li>
- +<li>spinal cord contusion<ul>
- +<li>thick high T2 signal rim around small central low T1 signal above or below level of trauma <sup>5</sup>
- +</li>
- +<li>blooming on T2* sequences</li>
-<li>contusion<ul><li>high T2 signal above or below level of trauma</li></ul>- +<li>intramedullary haemorrhage<ul>
- +<li>thin high T2 signal rim around large central low T1 signal <sup>5</sup>
-<li>swelling<ul><li>focal cord enlargement at level of trauma best seen on sagital T1</li></ul>- +<li>blooming on T2* sequences</li>
- +<li>see <a href="/articles/ageing-blood-on-mri">ageing blood on MRI</a> for other timescales</li>
- +</ul>
-<li>transection<ul><li>discontinuity of cord</li></ul>- +<li>spinal cord transection<ul><li>discontinuity of cord best seen on sagittal sequences</li></ul>
References changed:
- 2. Kirshblum SC, Burns SP, Biering-Sorensen F et-al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34 (6): 535-46. <a href="http://dx.doi.org/10.1179/204577211X13207446293695">doi:10.1179/204577211X13207446293695</a> - <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232636">Free text at pubmed</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/22330108">Pubmed citation</a><span class="auto"></span>
- 5. Mahmood NS, Kadavigere R, Avinash KR et-al. Magnetic resonance imaging in acute cervical spinal cord injury: a correlative study on spinal cord changes and 1 month motor recovery. Spinal Cord. 2008;46 (12): 791-7. <a href="http://dx.doi.org/10.1038/sc.2008.55">doi:10.1038/sc.2008.55</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/18542094">Pubmed citation</a><span class="auto"></span>
- 3. Katzberg RW, Benedetti PF, Drake CM et-al. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology. 1999;213 (1): 203-12. <a href="http://dx.doi.org/10.1148/radiology.213.1.r99oc40203">doi:10.1148/radiology.213.1.r99oc40203</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/10540663">Pubmed citation</a><span class="auto"></span>
- 4. Parizel PM, van der Zijden T, Gaudino S et-al. Trauma of the spine and spinal cord: imaging strategies. Eur Spine J. 2010;19 Suppl 1 (S1): S8-17. <a href="http://dx.doi.org/10.1007/s00586-009-1123-5">doi:10.1007/s00586-009-1123-5</a> - <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2899721">Free text at pubmed</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/19727855">Pubmed citation</a><span class="auto"></span>
Systems changed:
- Spine
- Trauma
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image 1 MRI (T2) ( create )

Image 2 MRI (T2 MEDIC) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.