Osteosarcoma
Updates to Article Attributes
Osteosarcomas are malignant bone forming tumours and the second most common primary bone tumour after multiple myeloma 4. They account for ~ 20~20% of all primary bone tumours 1,3,4.
Epidemiology
Osteosarcomas can be either primary or secondary, and these have differing demographics.
- primary osteosarcoma - typically occurs in young patients (10-20 years) with 75% occurring before the age of 20; which is logical because the growth centers of the bone are more active during the puberty to adolescence time period.3 Therefore the epidemiology can be easily understood. For less clear reasons, there is a slight male predominance.
- secondary osteosarcoma - occurs in the elderly, usually secondary to malignant degeneration of Paget's disease, extensive bone infarcts or post radiotherapy for other conditions.
Clinical presentation
Patients usually present with bone pain, occasionally accompanied by a soft-tissue mass or swelling. At times, the first symptoms are related to pathologic fracture.
The distribution of primary and secondary osteosarcomas is also different.
- primary tumours typically occur in the metaphyseal regions of long bones, and have a striking predilection for the knee, with up to 60% occurring there
- secondary tumours on the other hand, have a much wider distribution largely mirroring the combined incidence of their underlying condition, and thus much have a higher incidence in flat bones, especially the pelvis (a favourite site of Paget's disease)
Pathology
Osteosarcomas can be divided into a number of sub types according to degree of differentiation, location within the bone, and histological variants 3.
These sub types vary in imaging findings, demographics and biological behaviour, and include :
-
intramedullary ~ 80%
- conventional high-grade - most common and discussed in this article
- telangiectatic osteosarcoma
- low-grade osteosarcoma
- surface or juxtacortical ~ 10-15%
- extra skeletal ~ 5%
Macroscopically osteosarcomas are bulky tumours where a heterogeneous cut surface demonstrates areas of haemorrhage, fibrosis and cystic degeneration. Their extension within the medullary cavity is often much more extensive than the bulky part of the tumour would suggest. Areas of bone formation are characteristic of osteosarcomas, with the degree of bone formation varying widely.
Microscopically poorly formed trabecular bone is seen with (in the typical high grade conventional sub type) cellular pleomorphism and mitoses. Variable amounts fibrocytic and chondroblastic appearing cells may also be encountered.
Location
They typically occur at the metadiaphysis of tubular bones in the appendicular skeleton. Common sites include
- femur: ~ 40% (especially distal femur)
- tibia: ~ 16% (especially proximal tibia)
- humerus: ~ 15%
Other less common sites include
- fibula
- innominate bone
- mandible (gnathic osteosarcoma)
- maxilla
- vertebrae
Associations
- Paget's disease of bone
- irradiation
- Rothmund-Thomson syndrome
Markers
Serum alkaline phosphatase (ALP) may be raised (particularly with advanced disease)
Radiographic features
Plain film
Conventional radiography continues to play an important role in diagnosis. Typical appearances of conventional high grade osteosarcoma include:
- medullary and cortical bone destruction
- wide zone of transition, permeative or moth-eaten appearance
- aggressive periosteal reaction
- sunburst type
- Codman triangle
- lamellated (onionskin) reaction - less frequently seen
- soft-tissue mass
- tumour matrix ossification / calcification
- variable: reflects a combination of the amount of tumour bone production, calcified matrix, and osteoid
- ill-defined "fluffy" or "cloud-like" c.f to the rings and arcs of chondroid lesions
CT
The role of CT is predominantly in assisting biopsy and staging, but adds little to plain radiography and MRI in direct assessment of the tumour. The exception to this rule is predominantly lytic lesions in which small amounts of mineralized material may be inapparent on both plain film and MRI 4.
MRI
MRI is proving essential in accurate local staging and assessment for limb sparing resection, particularly for evaluation of intraosseous tumour extension and soft-tissue involvement. Assessment of the growth plate is also essential as up to 75 - 88% of metaphyseal tumours do cross the growth plate into the epiphysis 4.
-
T1
- soft tissue non-mineralized component : intermediate signal intensity
- mineralised / ossified components : low signal intensity
- peri-tumoural oedema : intermediate signal intensity
- scattered regions of haemorrhage will have variable signal (see ageing blood on MRI)
- enhancement : solid components enhance
-
T2
- soft tissue non-mineralized component : high signal intensity
- mineralised / ossified components : low signal intensity
- peri-tumoural oedema : high signal intensity
Treatment and prognosis
Work-up: local staging by MRI prior to biopsy and distant staging with bone scan and chest CT.
Cure, if achievable requires aggressive surgical resection often with amputation followed by chemotherapy. If a limb-salvage procedure is feasible, a course of multi-drug chemotherapy precedes surgery to downstage the tumour, followed by wide resection of the bone and insertion of an endoprosthesis. Currently, the 5-year survival rate after adequate therapy is approximately 60-80% 4.
The most frequent complications of conventional osteosarcoma are pathologic fracture and the development of metastatic disease, particularly to bone, lung and regional lymph nodes.
Differential diagnosis
General differential considerations include
When the lesion is at the posteromedial distal femur consider
-<p><strong>Osteosarcomas</strong> are malignant <a href="/articles/bone-forming-tumours-1">bone forming tumours</a> and the second most common primary bone tumour after <a href="/articles/multiple-myeloma-1">multiple myeloma</a> <sup>4</sup>. They account for ~ 20% of all primary bone tumours <sup>1,3,4</sup>.</p><h4>Epidemiology</h4><p>Osteosarcomas can be either primary or secondary, and these have differing demographics. </p><ul>- +<p><strong>Osteosarcomas</strong> are malignant <a href="/articles/bone-forming-tumours-1">bone forming tumours</a> and the second most common primary bone tumour after <a href="/articles/multiple-myeloma-1">multiple myeloma</a> <sup>4</sup>. They account for ~20% of all primary bone tumours <sup>1,3,4</sup>.</p><h4>Epidemiology</h4><p>Osteosarcomas can be either primary or secondary, and these have differing demographics. </p><ul>
Image ( update )
Image ( update )
Image ( update )
Image ( update )
Image ( create )
Image 2 Photo (Gross pathology) ( update )

Image 3 Pathology (H&E) ( update )

Image 4 MRI (T2) ( update )

Image 6 CT (bone window) ( update )

Image 7 X-ray (Frontal) ( update )

Image 8 X-ray (Frontal) ( update )

Image 9 X-ray (Lateral) ( update )

Image 10 MRI (T1 C+ fat sat) ( update )

Image 11 Nuclear medicine ( update )

Image 12 MRI (T1 C+ fat sat) ( update )

Image 13 X-ray (Frontal) ( update )

Image 14 CT (bone window) ( update )

Image 15 MRI (T1) ( update )
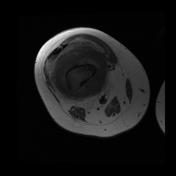
Image 16 CT (non-contrast) ( update )

Image 17 X-ray (Frontal) ( update )

Image 18 X-ray ( update )

Image 19 X-ray (Lateral) ( update )

Image 20 MRI (T1 C+) ( update )

Image 22 X-ray (Frontal) ( update )

Image 23 X-ray (Frontal) ( update )

Image 24 MRI (T1) ( update )

Image 25 CT (non-contrast) ( update )

Image 26 CT (C+ arterial phase) ( update )

Image 27 X-ray (Frontal) ( update )

Image 28 X-ray (Frontal) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.